This page is part of the Da Vinci Risk Adjustment FHIR Implementation Guide (v2.0.0-ballot: STU 2 Ballot) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.1.0. For a full list of available versions, see the Directory of published versions
All sections on this page are new content.
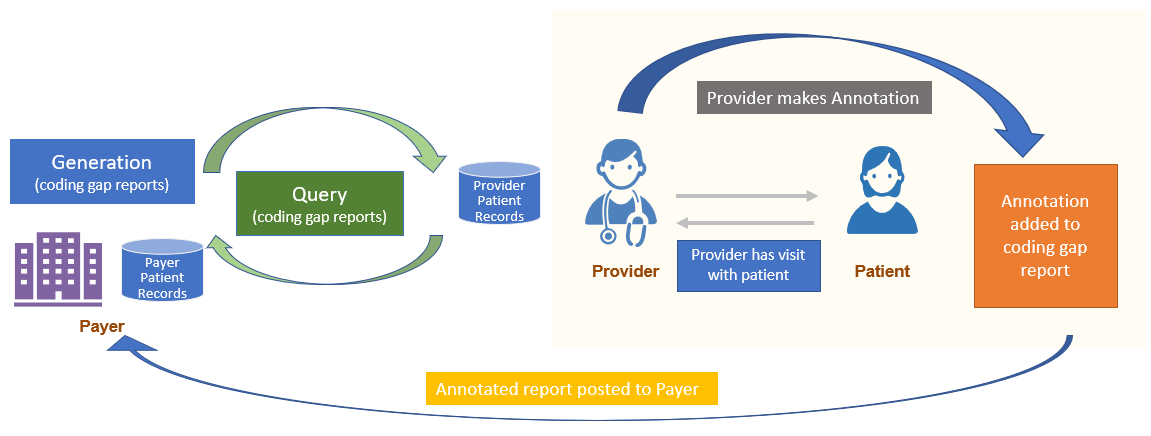
Systems may choose to display the Risk Adjustment Coding Gap Report to a Provider at the time of a patient’s care. When this happens, a Provider (using the Remediation Client role) may choose to annotate the report to let the Payer know they took some action in regard to the coding gap(s) when they saw the patient.
Note: Annotation is not intended to change the status of a Coding Category gap. The Remediation process using the Task Resource should be used instead. Note that both Annotation and Task can be generated at the time the Provider sees the patient if that is appropriate.
For annotation, there is an extension, called Annotation. This extension was added to the Risk Adjustment Coding Gap Report within the MeasureReport.group element. This allows for an annotation to specifically reference a Condition Category code. Also note the annotation is a Complex extension and can repeat. Within the annotation extension are several fields, all of which are optional:
annotator indicates who provided the annotation. It can link to a US Core Organization, a US Core Practitioner or a US Core PractitionerRole which allows you to reference both a Practitioner and an Organizationannotated when the annotation was madetext a free text annotationcode a coded annotation to indicate the specific action taken. The code list which is extensible includes acknowledged, assessed and not present, assessed and present, and deferredidentifier that can be used to link to a claim or document that the provider is sending via another method or transactionThe Provider’s system SHALL NOT change any other part of the original Risk Adjustment Coding Gap Report and can only add the Annotation to the appropriate MeasureReport.group(s). If a provider wants to share data with the Payer in order to change a gap status, they should use the Remediation process.
Once an Annotation is added to a Risk Adjustment Coding Gap Report, it can be posted to the Payer’s Reporting Server.
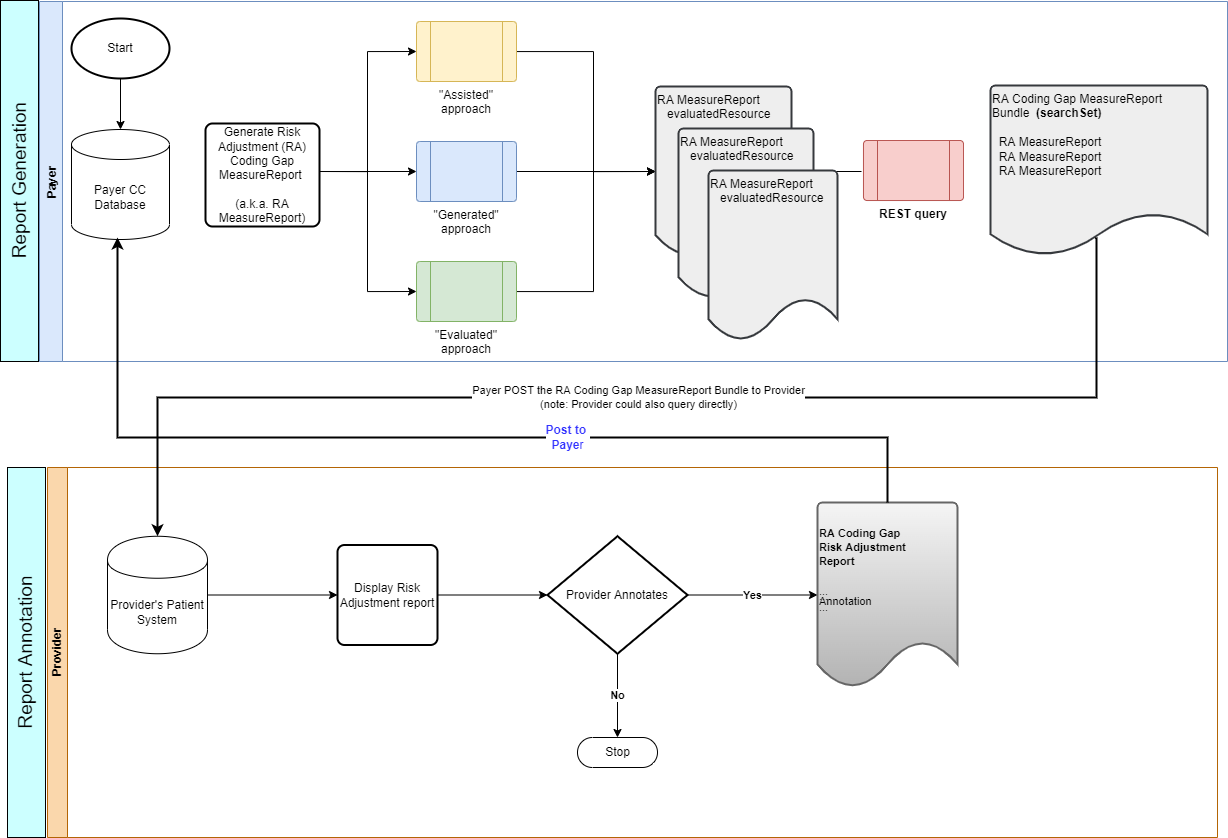
This implementation guide does not direct any action be taken by the Payer upon receipt of an annotated Risk Adjustment Coding Gap Report.
After a payer generates a subsequent Risk Adjustment Coding Gap Report, in their role as a Remediation Server can choose to include the annotations as they see fit. This might include adding the annotations only if received from the same Provider up to including all annotations they have received. The Payer is not required to include any annotations on subsequently generated Risk Adjustment Coding Gap Report.