This page is part of the Da Vinci Risk Adjustment FHIR Implementation Guide (v2.0.0-ballot: STU 2 Ballot) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.1.0. For a full list of available versions, see the Directory of published versions
The Da Vinci Project member organizations have identified the need of standardizing how risk adjustment coding gaps are communicated between payers and providers. This implementation guide (IG) specifies standardized risk adjustment coding gap reports and provides guidance to query the coding gap reports from Payer for one or more patients. Standardizing the reporting structure helps lessen the burden on the providers in processing the reports so they can more easily address the patients’ care needs. This standardized structure also supports the Payer sharing information that they have but the providers may not, such as data from other providers’ claims, lab results, filled prescriptions, etc.
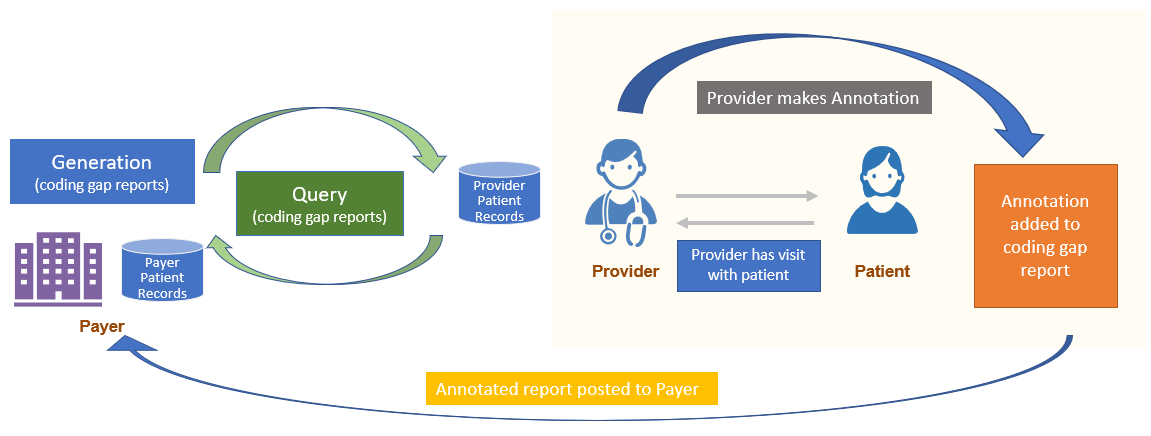
This IG also provides mechanisms enabling the feedback loop from Provider to Payer. Provider may add annotation on the Risk Adjustment Coding Gap Report that they took some action(s) for a specific coding gap on the report and communicates that back to the Payer. However, if Provider identifies a coding gap that is on the report needs to be closed or invalidated based on medical record review, this feedback process is done through the Task profile, Risk Adjustment Clinical Evaluation Evidence Task, which allows the Provider to send the supporting clinical evaluation evidence to the Payer. This feedback loop is important for achieving the goal of improving the accuracy and completeness of risk adjustment.
Figure 2.1-1 shows a high level overview of the risk adjustment workflow, which consists of three main phases: Report Generation, Report Query, and Remediation. Detailed guidance for each phase is provided on a seperate page under the Methodolody section.
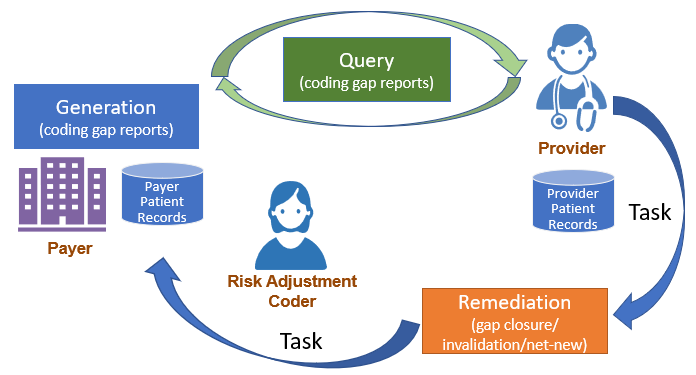
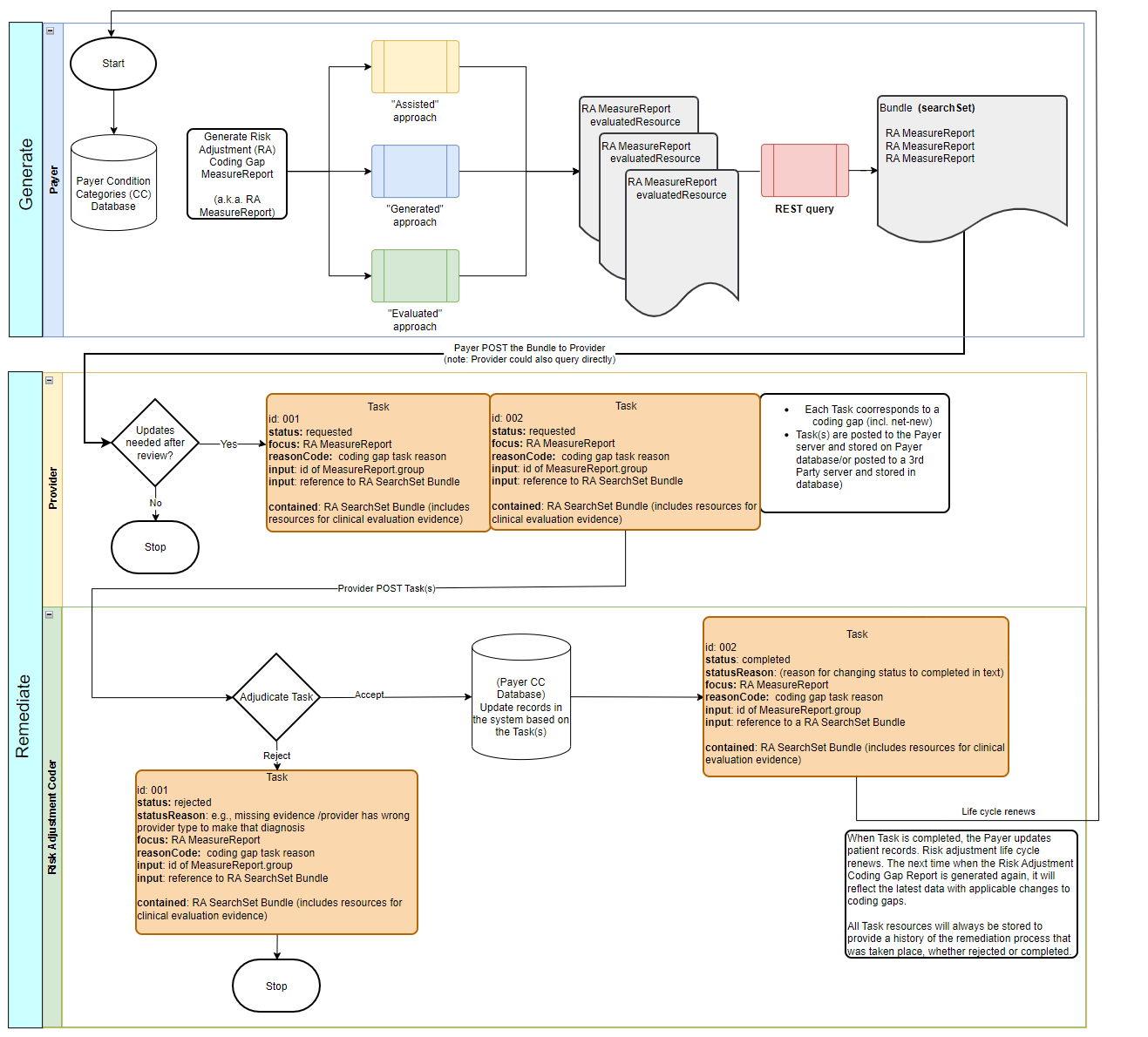
Report generation describes three different approaches to generate Risk Adjustment Coding Gap Report, which are referred to as Assisted, Generated, and Evaluated in this IG.
The Client can query the Risk Adjustment Coding Gap Report once they are generated. For example, Payer acts as the Reporting Client can query reports based on search parameters and POST them to the Provider server. See the Report Query page for details and guidance.
Once the queried Risk Adjustment Coding Gap MeasureReports have been sent to the intended recipient and filtered to ensure that only germane coding gaps (e.g., HCC gaps) are made available to providers. The Provider (or a software program acting on behalf of the Provider) determines whether the coding gap is currently valid, and whether the requested encounter data evidence exists to close the gap. The Provider will be able to use the functionalities specified in this IG to begin remediation process to request for a gap closure, gap invalidation, and/or addition of a net-new coding gap, and submits clinical evaluation evidence to support the request.
The remediation workflow is supported by using the Task resource, Risk Adjustment Clinical Evaluation Evidence Task. Remediation allows the Risk Adjustment Coder to validate evidence and adjudicate coding gap change requests through Task from the Provider. The updated Task is then posted to the Payer server and the records on the Payer system get updated accordingly.
See the Remediation page for more details and guidance.
The diagram below provides a workflow overview of the report generation, query, and remediation steps.
An electronical medical record (EMR) may choose to display all or part of the Risk Adjustment Coding Gap Report to the Provider at the point of care. At that time, if the Provider wants to note the action they took in regard to a Risk Adjustment coding gap, they can put that comment on the Risk Adjustment Coding Gap Report and return it to the Payer. This process is called Report Annotation.
Member attribution establishes associations between providers and payers. The process of establishing and exchanging patient lists for risk adjustment coding gap report is not in the scope of this implementation guide. One possible way of exchanging Member Attribution Lists between providers and payers is described in the Da Vinci - Member Attribution (ATR) List implementation guide.
Certain elements in the profiles defined in this implementation guide are marked as Must Support. This flag is used to indicate that the element plays a critical role in defining and sharing risk adjustment coding gaps, and implementations SHALL understand and process the element.
This implementation guide uses US Core profiles where appropriate, therefore, the implications of the Must Support flag for US Core profiles must also be considered.
For more information, see the definition of Must Support in the base FHIR specification.
This implementation guide relies on the following specifications: