This page is part of the Da Vinci Risk Adjustment FHIR Implementation Guide (v2.0.0-ballot: STU 2 Ballot) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.1.0. For a full list of available versions, see the Directory of published versions
All sections on this page are new content.
Once the Risk Adjustment Coding Gap Report has been constructed, it is sent to the intended recipient and filtered to ensure that only germane HCC gaps are made available to providers. The Provider (or a software program acting on behalf of the Provider) determines whether the gap is currently valid, and whether the requested encounter data evidence exists to close the gap. Three courses of action are available to the Provider (or a software program acting on behalf of the Provider):
Just as the Payer is responsible for generating HCC gaps, so too are they responsible for resolving them. The Payer ingests the gap closure and gap invalidation data supplied by the Provider and reviewed by the Risk Adjustment Coder, and formally updates the gap status. It is recommended that the Payer record the date when the gap status change occurs so that providers may receive credit for their performance (e.g., if the Payer incentivizes providers for early closure of HCC gaps prior to the Medicare Advantage September sweeps.) At this time the Payer will perform any necessary backend processes before closing the loop with the generation of a new HCC gap list, and the cycle begins anew. While these payer backend processes are largely outside the scope of this implementation guide (IG), there are times when they can impact gap data. One of these is the process of submitting risk adjustment data to government agencies (e.g., Encounter Data Processing System (EDPS) in the case of MA risk adjustment; the Edge Server in the case of ACA risk adjustment.) It is possible that an HCC gap closure may not be confirmed by these agencies during the submission process, either because the HCC is rejected or because of a submission error. Either way, a situation may arise whereby the HCC gap is closed from the Payer’s perspective, but the data has not been accepted from the government’s perspective. This can place the Payer in a quandary, since the Risk Adjustment IG recommends that the Payer close the loop by sending the Provider confirmation that their gap closure or invalidation request has been processed. If the Payer provides this confirmation, then the government agency subsequently rejects the encounter data submission, the Payer might need to reopen the HCC gap – and this can lead to provider abrasion. It is up to the Payer to decide how to handle this situation, but the Risk Adjustment IG has provided an additional evidenceStatus value of pending to indicate to the Provider that the Payer has received their gap closure request, and is in the process of confirming that closure with the government agency. The Payer will subsequently change the evidenceStatus to open-gap or closed-gap depending on the resolution of that submission.
The Actors involved in the remediation phase are Provider, Risk Adjustment Coder, and Payer.
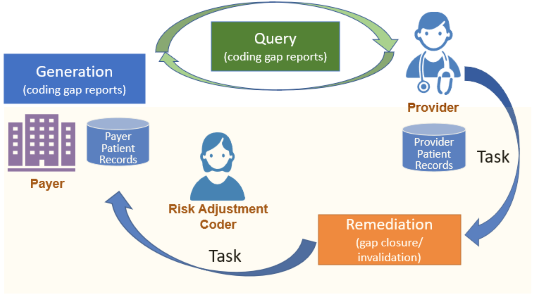
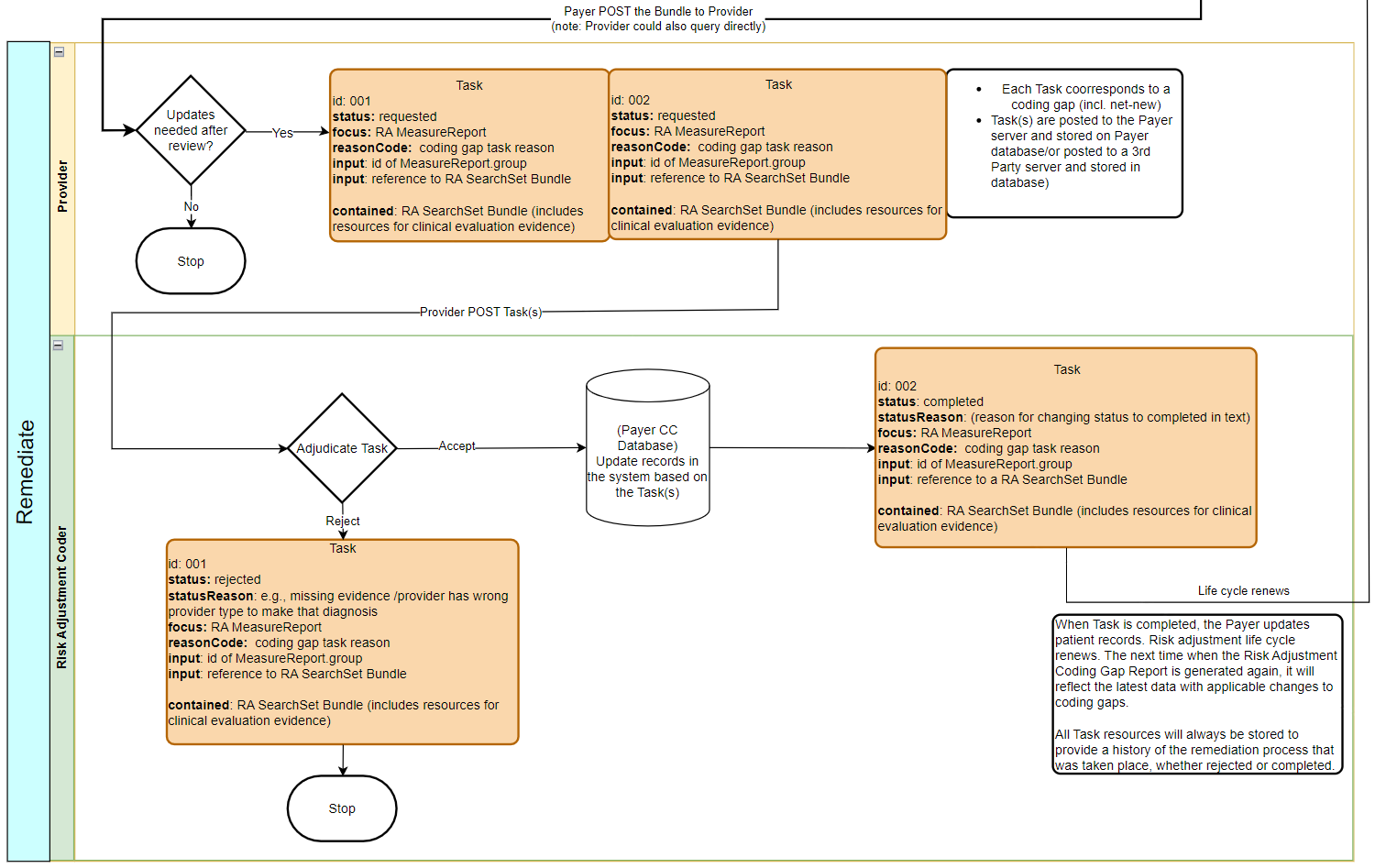
Figure 2.4-1 provides an overview of how the Task resource, Risk Adjustment Clinical Evaluation Evidence Task, is used to support the remediation process. The Task State Machine includes a diagram for the state machine used by this profile.
After the Report Query step, the Provider reviews the coding gaps and determines whether they need to initiate the gap closure/invalidation process based on the clinical evaluation evidence after the review.
Task.status to requestedTask.focus to reference the Risk Adjustment Coding Gap Report resource that contains the Condition Category code (a.k.a, HCC) that this Task is forTask.reasonCode using an appropriate code, such as closure-request or invalidation-request-never-had-condition, from the Coding Gap Task Reason ValueSet. Use the code creation-request for net-new. This is the reason for providing clinical evaluation evidence.Task.input with MeasureReport.group.id as value
Task.reasonCode is other than creation, then a Task must have an input with MeasureReport.group.id as value. For example, the input.value is the group.id for HCC189 from the MeasureReport. MeasureReport.group.id uniquely identifies a Condition Category code that is included in a MeasureReport, this is how to indicate in Task which coding gap (a.k.a, HCC) the Task is for.Task.input to reference a Risk Adjustment SearchSet Bundle
Task.input references a searchSet Bundle, the Risk Adjustment SearchSet Bundle, which is a contained resource of this Task.Task.contained contains the searchSet Bundle resource
Task.contained. The searchSet Bundle includes entries for resources of clinical evaluation evidence and the absolute url of these resources which are provided in Bundle.entry.fullUrl. For example, if the Provider provides an Encounter and a Condition resources as clinical evaluation evidence, the Task will have a Task.input references a searchSet Bundle with two entries, one entry with the Encounter resource with its fullUrl and the other entry with the Condition resource with its fullUrl.Provider posts (POST) the Task resource (in a requsted status) to the Payer or a 3rd Party Server for review by the Risk Adjustment Coder. The Risk Adjustment Coder reviews the Task and the contained clinical evaluation evidence and conducts medical record review.
The Risk Adjustment Coder has option to either reject or complete a Task.
Task.status from requsted to rejectedstatusReason.textTask.lastModified timestamprequested to completed and the lastModified is also updated.The risk adjustment lifecycle renews. The risk adjustment engine runs against the patient records with the updated information. The generated Risk Adjustment Coding Gap MeasureReports would then reflect more accurate and up-to-date coding gap information. Note that Provider sending a Task for change request, for example a closure request, would not guarantee a gap closure on the Payer end.
These Task resources should be stored, so the Provider, the Risk Adjustment Coder, or the Payer can access them and be able to review Tasks details and their updates history made throughout the lifecyle.