Publication Build: This will be filled in by the publication tooling
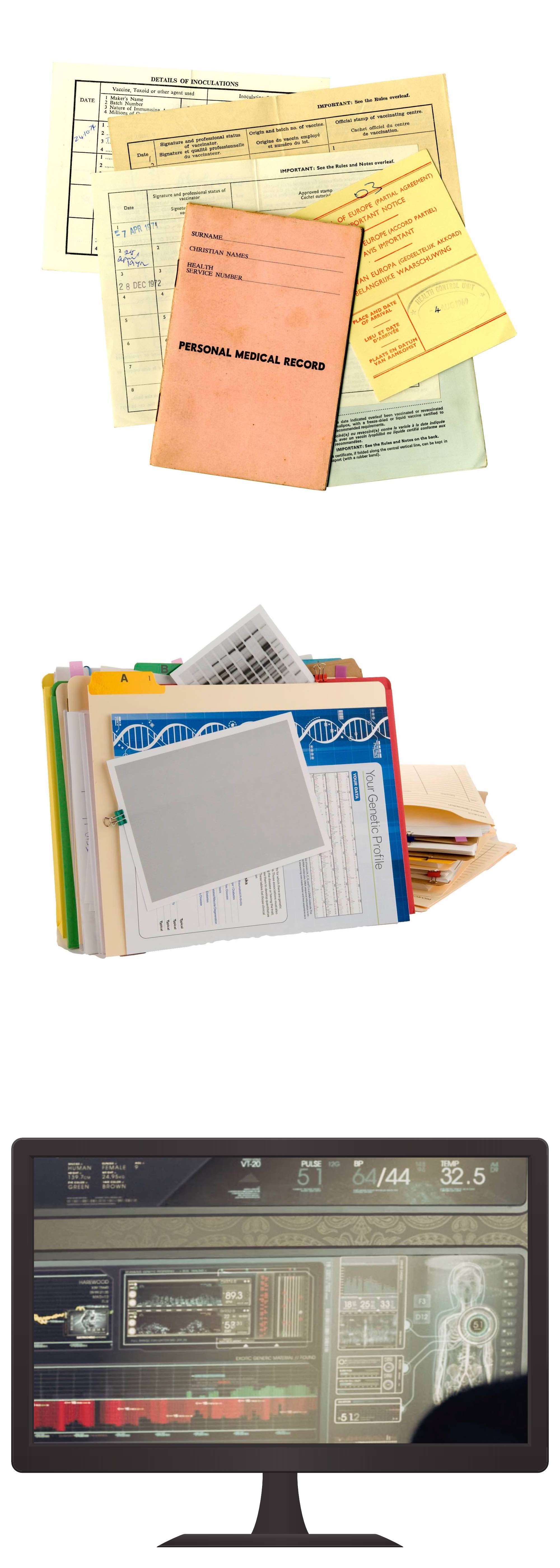
Medical records have been around since as long as there have been practicing physicials. Modern medical record systems began in 1665, however, with the Bills of Mortality of London, England, which eventually became the Internal Clasification of Diseases, and defined a standard Code System for recording diseases. Later, advances in library science led to the adoption of record keeping conventions, such as the Dewey Decimal System and the Card Catalog patent.
In 1945, the Enigma Project invented the first digital computer, to which library science information management principles were soon added. By 1970, digital computers became accessible enough that hospitals could use them to track patient visits for accounting purposes, which led to the assachusetts General Hospital Utility Multi-Programming System (MUMPS/VAX), which is commonly regarded as the first electronic medical record system.
Soon after, the personal computing revolution saw the general population become able to purchase a home computer, and with it a flury of patients using these PCs to manage their personal health using spreadsheets and small self-written offline medical record management utilities.
Many of these utilities were eventually abandoned; but others found themselves in a process of consolidation and gravitating towards what would eventually become the major electronic medical record vendors (i.e. Meditech, Epic, Cerner, Allscripts, etc).
Eventually these systems had need to exchange information with each other, and an era of point-to-point communication was begun using HL7 v2. After nearly 3 decades of this approach, the need to renegotiate interfaces between every business partner eventually lead to the development of reusable data endpoints, as described by Fast Healthcare Interoperability Resources (FHIR).
This web-standards based protocol has been widely adopted by clinicians and industry technology vendors. And in the mid 2010s, laws in the United States and elsewhere began being passed requiring the use of interoperability standards; with one notable example being the U.S. 21st Century Cures Act, which formalized patient rights to access their own data using standardized interoperability protocols.
This changed legal environment has created an opportunity for a new ecosystem of applications, products, and services that incorporate patient health records; with early adopter organizations such as MyLinks, MaxMD, Symptomatic, and 1Up Health advocating on behalf of patients and their rights under the 21st Century Cures law.