This page is part of the US-Medication FHIR IG (v1.1.0: STU 2 Ballot 1) based on FHIR R3. The current version which supercedes this version is 1.2.0. For a full list of available versions, see the Directory of published versions 
In the United States, every state is deploying a Prescription Drug Monitoring Program (PDMP) which track controlled substance prescriptions within the state. Overtime, these PDMP databases start to provide rich information on provider and patient behaviors with respect to prescribing and use of controlled substances. Enabling a Provider to access a Patient’s PDMP data during care delivery will help in avoiding potential drug misuse, abuse and diversion also commonly known as Opioid abuse. In order to reduce opioid abuse, some states have implemented policies mandating Providers to check the state PDMP for the Patient’s controlled substance history before prescribing any controlled substances. To further address opioid abuse which is a current national priority, the US Meds Prescription Drug Monitoring Program FHIR Implementation Guide (US Meds PDMP FHIR IG) outlines how systems can access PDMP data for a patient from the state PDMP systems using the HL7 FHIR standard. For general background on state PDMPs, see the Centers for Disease Control and Prevention what states need to know about PDMPs.
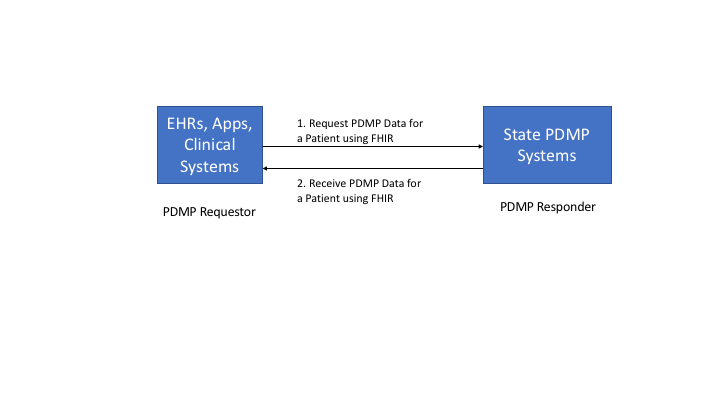
This section outlines the transactions which are in-scope and not in-scope for the US Meds PDMP FHIR IG. As shown in the Figure 1 below, the PDMP eco-system can be simplified for the purpose of this project to consist of EHRs or Clinical Systems, Pharmacies and the State PDMP systems.
The US Meds PDMP FHIR IG defines how an EHR or an App or other Clinical Systems can access a Patient’s controlled substance prescription history from the State PDMP systems. This is identified by Interaction 3 in the diagram. All other interactions such as Interaction 1 and 2 in the diagram below are important for the overall PDMP eco-system, they are not in-scope for this project and IG.

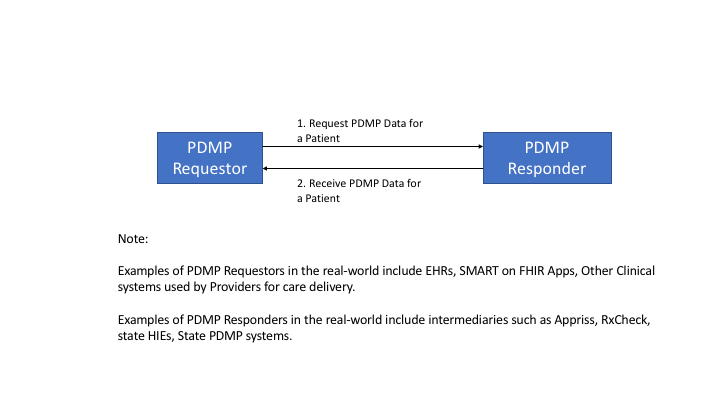
This section defines the abstract model which is used to identify the specific actors and interactions that are in-scope for the project. The abstract model is as shown in Figure 2 below which consists of two actors namely the PDMP Requestor and the PDMP Responder.
PDMP Requestor: PDMP Requestor is a health IT system that is requesting a Patient’s controlled substance history. Real-world examples of such health IT systems include EHRs, SMART on FHIR Apps and other Clinical Systems used for care delivery.
PDMP Responder: PDMP Responder is a health IT system that accepts a request from a PDMP Requestor and responds to the request with a controlled substance history for the patient. Real-world examples of such health IT systems include intermediary gateways such as Appriss, RxCheck, State HIEs and State PDMP systems.
Note: PDMP Responders which are acting as intermediaries provide additional value add services such being able to query multiple State PDMP systems, analytics which provide additional information for the Provider requesting the information. The fact that a PDMP Responder is an intermediary or if it is the actual State PDMP system is transparent to the PDMP Requestor and is more of a deployment architecture.
The abstract model interactions can be implemented using FHIR in multiple ways namely
These APIs are discussed further in the next few sub-sections.
The FHIR standard provides a rich set of search mechanisms by which specific FHIR resources can be accessed from a FHIR server. Typically the search parameters are specified in the RESTful URL and accessed using the HTTP GET operation.
The following is an example of how search parameters will be used by a PDMP Requestor to retrieve PDMP data from a PDMP Responder.
GET [base]/MedicationDispense?subject:Patient.name.given=peter&subject:Patient.name.family=jacobs&subject:Patient.birthdate=eq1973-11-25&authorizingPrescription.dispenseRequest.validityPeriod=ge2010-01-01&authorizingPrescription.dispenseRequest.validityPeriod=le2015-12-31&_include=MedicationDispense:subject&_include:recurse=MedicationDispense:authorizingPrescription&_include=MedicationDispense:medication
The above API will fetch all MedicationDispense resources for Patient with a given name of “peter” and family name of “jacobs” with a birthdate of “1973-11-25” with a prescription that falls within in a 5 year window starting from January 1st 2010 to December 31st 2015 and as part of the returned information will include MedicationDispense, MedicationRequest, Practitioner, Organization, Patient and Medication information as part of the returned bundle.
Also as part of the Search API one can specify to the server to include additional information such as the prescriber information, patient information. The combinations that need to be implemented by the US Meds PDMP FHIR IG actors will be described in detail as part of the Capability Statements.
The FHIR standard also provides APIs that resemble messaging paradigm similar to HL7 v2. These are part of the FHIR Messaging APIs. A PDMP Requestor can request prescription history for a patient by invoking the $process-message on the base URL as follows:
POST [base-url]/$process-message
NOTE: FHIR Messaging APIs will require the use of the POST operation even to access data.
The body of the message will be a FHIR Bundle that contains a MessageHeader resource as the first entry with the following minimum details:
The PDMP Responder has to be able to process this message and return back a Bundle which contains all the MedicationDispense resources along with Practitioner, Organization and Patient resources related to the data set. In case of errors OperationOutcome would be returned similar to any regular FHIR API.
NOTE: FHIR Messaging operations can only be invoked on FHIR Servers which conform to the FHIR Messaging operations in their capability statements and not on regular FHIR servers implementing RESTful Search APIs.
For the purposes of the US Meds PDMP FHIR IG, the FHIR Search APIs will be used and will be specified in detail in the CapabilityStatements for the actors. While both the Search and Messaging APIs have their own strengths and weaknesses, the decision to use FHIR Search APIs is based on the following factors
All implementers of FHIR servers and clients should pay attention to FHIR Security considerations. In addition to the FHIR Security considerations, the PDMP requests need to contain specific information about Requestor Identity and Requestor Facility information. Providing this information using FHIR Search APIs is very cumbersome and is not necessary. This kind of information can be collected by the PDMP Responder’s Authorization Server during application registration and avoid repeating the information on each request. These mechanisms are outlined in great detail in the SMART Backend Services Authorization Guide. The US Meds PDMP FHIR IG will use the SMART Backend Services Authorization Guide to collect the necessary requestor information appropriate to making the PDMP data request. In addition the authentication and authorization mechanisms will be used as part of requesting the PDMP data using the FHIR Search APIs.
This section describes identifies data elements that are used commonly in the PDMP data requests and responses and provides mappings of these data elements to FHIR. Based on environmental scans and prior performed by ONC across a spectrum of PDMP implementations the following data was collected:
Based on the above findings, NCPDP Request and Response data elements have been used as a starting point to specify the FHIR APIs. Since the community understands these NCPDP data elements, a mapping of NCPDP Request and Response data elements to FHIR Resources has been created and specified below. This allows organizations already familiar with NCPDP to use the mapping provided to develop their FHIR Resources and APIs. Similarly mapping from PMIX/NIEM data elements to FHIR is also provided for systems using PMIX/NIEM to map their data to FHIR and expose them through appropriate APIs.
This section includes the minimal mapping for the PDMP request from an EHR to a state PDMP using NCPDP.
| PDMP Request Data Element | NCPDP Data Element | FHIR Data Element | |
| Routing Information | |||
| Request | Requestor | <Last Name> <First Name> | Practitioner.name |
| Requestor Role | <Qualifer> | PractitionerRole.code | |
| Request ID | <MessageID> | MessageHeader.id | |
| Request date/ timestamp | <SentTime> | MessageHeader.timestamp | |
| Requestor Identifier | NPI Number* | <NPI> | Practitioner.identifier |
| DEA Number* | <DEANumber> | Practitioner.identifier | |
| Requesting Facility ID | DEA Number* | <DEANumber> | Organization.identifier |
| NCPDP Number* | <NCPDPID> | Organization.identifier | |
| NPI* | <NPI> | Organization.identifier | |
| Requesting Faciltiy | Facility Name | <Store Name> <Clinic Name> | Organization.name |
| State code of Requesting Facility | <State> | Organization.address | |
| Message Body | |||
| Patient | First Name | <FirstName> | MedicationDispense.subject(Patient) --> Patient.name.given |
| Last Name | <LastName> | MedicationDispense.subject(Patient) --> Patient.name.family | |
| Date of Birth | <DateofBirth> | MedicationDispense.subject(Patient) --> Patient.birthdate | |
| Request Prescription Date Range | Start Date | <EffectiveDate> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod |
| End Date | <ExpirationDate> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod | |
| Conditionally required data elements have .maptable1terisks (*), meaning at least one data element .maptable1 required within its category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) .maptable1 required. | |||
This section includes the minimal mapping for the PDMP response from a state PDMP to an EHR using NCPDP.
| PDMP Response Data Element | NCPDP Data Element | FHIR Data Element | |
| Routing Information | |||
| Response Date/ Timestamp | <SentTime> | MessageHeader.timestamp | |
| Response Prescription Date Range (Start Date) | <EffectiveDate> | MessageHeader | |
| Response Prescription Date Range (End date) | <ExpirationDate> | MessageHeader | |
| Request ID | <RelatesToMessageID> | MessageHeader.response.identifier | |
| Message Body | |||
| Patient | Patient First Name | <FirstName> | Patient.name.given |
| Patient Last Name | <LastName> | Patient.name.family | |
| Patient Date of Birth | <DateOfBirth> | Patient.birthdate | |
| Patient Gender | <Gender> | Patient.gender | |
| Patient Street Address | <AddressLine> <AddressLine2> | Patient.address.line | |
| Patient City Address | <City> | Patient.address.city | |
| Patient State Code | <State> | Patient.address.state | |
| Patient Zip Code | <ZipCode> | Patient.address.potalCode | |
| Patient Identifier | SSN* | <SocialSecurity> | Patient.identifier |
| Prescription | Prescription Filled Date | <LastFillDate> | MedicationDispense.whenPrepared |
| Prescription Written Date | <WrittenDate> | MedicationDispense.authorizingPrescription.authoredOn | |
| Prescription Number | <SourceReference> | MedicationDispense.Identifier | |
| Drug Name[1] | <DrugDescription> | MedicationDispense.medication[x] | |
| Drug Strength[1] | <StrengthValue, Code> fields | Medication.ingredient.itemReference | |
| Dosage Form[2] | <FormCode> | Medication.form | |
| Drug Quantity | <Quantity> | MedicationDispense.quantity | |
| Days of Supply | <DaysSupply> | MedicationDispense.daysSupply | |
| Refill Number | <FillNumber> | Medication.request - extension | |
| Refills Authorized | <Refills> | MedicationDispense.authorizingPrescription.dispenseRequest.numberOfRepeatsAllowed | |
| Partial Fill Indicator | gap | MedicationDispense.type | |
| Method of Payment | <Note> | MedicationDispense.note | |
| Drug | Product ID Qualifier | <CodeListQualifier> | MedicationDipense.medicationCodeableConcept.code.system |
| Product ID | <ProductCode> | MedicationDispense.medicationCodeableConcept.code.value | |
| Dispenser Organization | Dispenser Organization Name (Facility) | <StoreName> | Organization.name |
| Dispenser Organization Street Address | <AddressLine> <AddressLine2> | Organization.address.line | |
| Dispenser Organization City Address | <City> | Organization.address.city | |
| Dispenser Organization State Code | <State> | Organization.address.state | |
| Dispenser Organization Zip Code | <ZipCode> | Organization.address.potalCode | |
| Dispenser Organization Phone Number | <CommunicationNumber> | Organization.telecom | |
| Dispenser Organization (Pharmacy identifier) | DEA Number* | <DEANumber> | Organization.identifier |
| NCPDP Number* | <NCPDPID> | Organization.identifier | |
| NPI Number* | <NPI> | Organization.identifier | |
| Prescriber | Prescriber First Name | <FirstName> | Practitioner.name.given |
| Prescriber Last Name | <LastName> | Practitioner.name.family | |
| Prescriber Street Address | <AddressLine> <AddressLine2> | Practitioner.address.line | |
| Prescriber City Address | <City> | Practitioner.address.city | |
| Prescriber State Code | <State> | Practitioner.address.state | |
| Prescriber Zip Code | <ZipCode> | Practitioner.address.potalCode | |
| Prescriber Identifier | DEA Number* | <DEANumber> | Practitioner.identifier |
| NPI Number* | <NPI> | Practitioner.identifier | |
| State License* Identifier | NA | Practitioner.identifier | |
| State of License* | NA | Practitioner.identifier | |
| *Conditionally required data elements have .maptable2terisks (*), meaning at least one data element .maptable2 required within its category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) .maptable2 required. | |||
This section includes the minimal mapping for the PDMP request from an EHR to a state PDMP using PMIX.
| PDMP Request Data Element | PMIX Data Element | FHIR Data Element | |
| Routing Information | |||
| Request | Requestor | <pmix:Requestor> | Practitioner.name |
| Requestor Role | <pmix:RequestorRole> | PractitionerRole.code | |
| Request ID | <pmix:RequestID> | MessageHeader.id | |
| Request date/ timestamp | n/a | MessageHeader.timestamp | |
| Requestor Identifier | NPI Number* | <nc:IdentificationID> | Practitioner.identifier |
| DEA Number* | <nc:IdentificationID> | Practitioner.identifier | |
| Requesting Facility ID | DEA Number* | <nc:IdentificationID> | Organization.identifier |
| NCPDP Number* | <nc:IdentificationID> | Organization.identifier | |
| NPI* | <nc:IdentificationID> | Organization.identifier | |
| Requesting Faciltiy | Facility Name | <nc:OrganizationDoingBusinessAsName> | Organization.name |
| State code of Requesting Facility | <nc:LocationStateUSPostalServiceCode> | Organization.address | |
| Message Body | |||
| Patient | First Name | <nc:PersonGivenName> | MedicationDispense.subject(Patient) --> Patient.name.given |
| Last Name | <nc:PersonSurName> | MedicationDispense.subject(Patient) --> Patient.name.family | |
| Date of Birth | <nc:Date> | MedicationDispense.subject(Patient) --> Patient.birthdate | |
| Request Prescription Date Range | Start Date | <pmp:RequestPrescriptionDateRangeBegin> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod |
| End Date | <pmp:RequestPrescriptionDateRangeEnd> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod | |
| Conditionally required data elements have .maptable1terisks (*), meaning at least one data element .maptable1 required within its category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) .maptable1 required. | |||
This section includes the minimal mapping for the PDMP response from a state PDMP to an EHR using PMIX.
| PDMP Response Data Element | NCPDP Data Element | FHIR Data Element | |
| Routing Information | |||
| Response Date/ Timestamp | <pmp:ReportExecutionDate><pmp:ReportExecutionTime> | MessageHeader.timestamp | |
| Response Prescription Date Range (Start Date) | <pmp:ReportDateRangeBegin> | MessageHeader | |
| Response Prescription Date Range (End date) | <pmp:ReportDateRangeEnd> | MessageHeader | |
| Request ID | n/a | MessageHeader.response.identifier | |
| Message Body | |||
| Patient | Patient First Name | <nc:PersonGivenName> | Patient.name.given |
| Patient Last Name | <nc:PersonSurName> | Patient.name.family | |
| Patient Date of Birth | <nc:Date> | Patient.birthdate | |
| Patient Gender | <PersonSexCode> | Patient.gender | |
| Patient Street Address | <StreetFullText> | Patient.address.line | |
| Patient City Address | <nc:LocationCityName> | Patient.address.city | |
| Patient State Code | <nc:LocationStateUSPostalServiceCode> | Patient.address.state | |
| Patient Zip Code | <nc:LocationPostalExtensionCod> | Patient.address.potalCode | |
| Patient Identifier | SSN* | <nc:IdentificationID> | Patient.identifier |
| Prescription | Prescription Filled Date | <pmp:ReportDateRangeBegin><pmp:ReportDateRangeEnd> | MedicationDispense.whenPrepared |
| Prescription Written Date | <nc:Date> | MedicationDispense.authorizingPrescription.authoredOn | |
| Prescription Number | <pmp:PrescriptionNumberText> | MedicationDispense.Identifier | |
| Drug Name[1] | <pmp:DrugProductNameText> | MedicationDispense.medication[x] | |
| Drug Strength[1] | <pmp:DrugStrengthText> | Medication.ingredient.itemReference | |
| Dosage Form[2] | <pmp:DrugUnitOfMeasureText> | Medication.form | |
| Drug Quantity | <pmp:DispensedQuantity> | MedicationDispense.quantity | |
| Days of Supply | <pmp:DaysSupplyCount> | MedicationDispense.daysSupply | |
| Refill Number | <pmp:DrugRefillNumberCount> | Medication.request - extension | |
| Refills Authorized | <pmp:RefillsAuthorizedCount> | MedicationDispense.authorizingPrescription.dispenseRequest.numberOfRepeatsAllowed | |
| Partial Fill Indicator | <pmp:PartialFillIndicator> | MedicationDispense.type | |
| Method of Payment | <pmp:MethodOfPaymentCode> | MedicationDispense.note | |
| Drug | Product ID Qualifier | <pmp:DrugCPDProductIdentifier><pmp:DrugDINProductIdentifier></br><pmp:DrugHRIProductIdentifier><pmp:pmp:DrugNDCProductIdentifier></br><pmp:DrugUPCProductIdentifie><pmp:DrugUPNProductIdentifier> | MedicationDispense.medicationCodeableConcept.code.system |
| Product ID | <IdentificationID> | MedicationDispense.medicationCodeableConcept.code.value | |
| Dispenser Organization | Dispenser Organization Name (Facility) | <nc:OrganizationDoingBusinessAsName> | Organization.name |
| Dispenser Organization Street Address | <nc:StreetFullText> | Organization.address.line | |
| Dispenser Organization City Address | <nc:LocationCityName> | Organization.address.city | |
| Dispenser Organization State Code | <nc:LocationStateUSPostalServiceCode> | Organization.address.state | |
| Dispenser Organization Zip Code | <nc:LocationPostalCode> | Organization.address.potalCode | |
| Dispenser Organization Phone Number | <nc:TelephoneNumberFullID> | Organization.telecom | |
| Dispenser Organization (Pharmacy identifier) | DEA Number* | <nc:IdentificationIDgt; | Organization.identifier |
| NCPDP Number* | <nc:IdentificationID> | Organization.identifier | |
| NPI Number* | <nc:IdentificationID> | Organization.identifier | |
| Prescriber | Prescriber First Name | <nc:PersonGivenName> | Practitioner.name.given |
| Prescriber Last Name | <nc:PersonSurName> | Practitioner.name.family | |
| Prescriber Street Address | <nc:StreetFullText> | Practitioner.address.line | |
| Prescriber City Address | <nc:LocationCityName> | Practitioner.address.city | |
| Prescriber State Code | <nc:LocationStateUSPostalServiceCode> | Practitioner.address.state | |
| Prescriber Zip Code | <LocationPostalCode> | Practitioner.address.potalCode | |
| Prescriber Identifier | DEA Number* | <IdentificationID> | Practitioner.identifier |
| NPI Number* | <IdentificationID> | Practitioner.identifier | |
| State License* Identifier | IdentificationID | Practitioner.identifier | |
| State of License* | IdentificationID | Practitioner.identifier | |
| *Conditionally required data elements have .maptable2terisks (*), meaning at least one data element .maptable2 required within its category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) .maptable2 required. | |||
This project does not create any new profiles, but will reuse the US-Core profiles and the US Meds profiles to request and receive PDMP data using FHIR resources.
This section identifies the CapabilityStatements defined for this implementation guide. The section outlines conformance requirements for each of the US Meds PDMP FHIR IG actors which includes the specific profiles, operations, security mechanisms and search parameters that need to be supported.
Note: The individual profiles identify the structural constraints, terminology bindings and invariants.
The section describes the expected capabilities of the PDMP Responder actor which is responsible for providing responses to the queries submitted by the PDMP Requestor applications.
The PDMP Responder SHALL:
The PDMP Responder SHOULD:
The PDMP Responder MAY:
The PDMP Responder SHALL support the FHIR Search interaction for MedicationDispense profile.
The PDMP Responder SHOULD support the FHIR Read profile interaction MedicationDispense profile.
The PDMP Responder MAY support other FHIR profile interactions.
The PDMP Responder SHALL support the SMART Backend Services Authorization Guide for verifying authentication and providing authorization to PDMP Requestors.
The PDMP Responder SHALL support the HTTP Header parameter X-Request-ID for request coorelation between the PDMP Requester and PDMP Responder.
The PDMP Responder SHALL support the following search parameters and combination for the MedicationDispense resource
The PDMP Responder SHALL support the following _include parameters for the MedicationDispense Search operations
The following is an example of the query.
GET [base]/MedicationDispense?subject:Patient.name.given=peter&subject:Patient.name.family=jacobs&subject:Patient.birthdate=eq1973-11-25&authorizingPrescription.dispenseRequest.validityPeriod=ge2010-01-01&authorizingPrescription.dispenseRequest.validityPeriod=le2015-12-31&_include=MedicationDispense:subject&_include:recurse=MedicationDispense:authorizingPrescription&_include=MedicationDispense:medication
The above API will fetch all MedicationDispense resources for Patient with a given name of “peter” and family name of “jacobs” with a birthdate of “1973-11-25” with a prescription that falls within in a 5 year window starting from January 1st 2010 to December 31st 2015 and as part of the returned information will include MedicationDispense, MedicationRequest, Practitioner, Organization, Patient and Medication information as part of the returned bundle.
All other information required to authenticate and authorize a PDMP Requestor is captured as part of registering the PDMP Requestor following the SMART Backend Services Authorization Guide.
The section describes the expected capabilities of the PDMP Requestor actor which is responsible for providing responses to the queries submitted by the PDMP Requestor applications.
The PDMP Requestor SHALL:
The PDMP Requestor SHOULD:
The PDMP Requestor SHALL support the FHIR Search interaction for MedicationDispense profile.
The PDMP Requestor SHOULD support the FHIR Read profile interaction for MedicationDispense profile.
The PDMP Requestor MAY support other FHIR profile interactions.
The PDMP Requestor SHALL support the SMART Backend Services Authorization Guide applicable to clients.
The PDMP Requestor SHALL add the HTTP Header parameter X-Request-ID as part of the Search request for request coorelation between the PDMP Requester and PDMP Responder.
The PDMP Requestor SHALL invoke the Search operation on the PDMP Responder including the following search and _include parameters when requesting PDMP data using the MedicationDispense resource
The PDMP Requestor SHALL include the following _include parameters for the MedicationDispense Search operations
The following is an example of the query.
GET [base]/MedicationDispense?subject:Patient.name.given=peter&subject:Patient.name.family=jacobs&subject:Patient.birthdate=eq1973-11-25&authorizingPrescription.dispenseRequest.validityPeriod=ge2010-01-01&authorizingPrescription.dispenseRequest.validityPeriod=le2015-12-31&_include=MedicationDispense:subject&_include:recurse=MedicationDispense:authorizingPrescription&_include=MedicationDispense:medication
The above API will fetch all MedicationDispense resources for Patient with a given name of “peter” and family name of “jacobs” with a birthdate of “1973-11-25” with a prescription that falls within in a 5 year window starting from January 1st 2010 to December 31st 2015 and as part of the returned information will include MedicationDispense, MedicationRequest, Practitioner, Organization, Patient and Medication information as part of the returned bundle.
The US Meds PDMP FHIR IG does not add any patient matching requirements to the PDMP actors, but relies on existing practices used for patient matching based on the first name, last name and date of birth provided through the request.
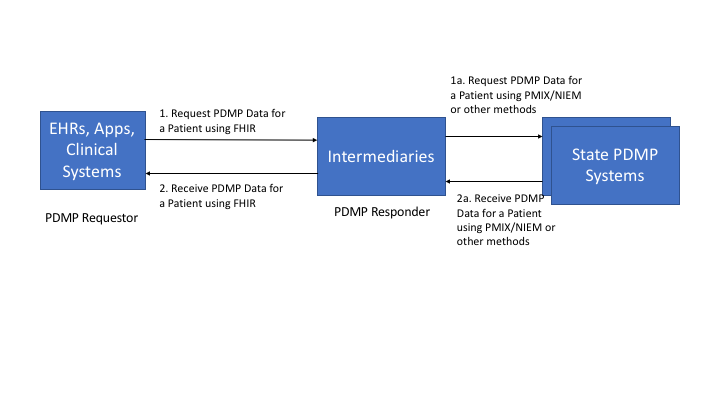
The following are deployment options showing how the US Meds PDMP FHIR IG can be used to implement the various actors.
In this deployment option, the EHRs, Apps and Clinical Systems act as the PDMP Requestors and interact with Intermediary Gateways such as Appriss, RxCheck which act as the PDMP Responders. The communication is performed using FHIR APIs. In this case the PDMP Requestors are isolated from the State PDMP Systems and the protocols they support.
The Intermediaries may translate the incoming FHIR request for data to a PMIX/NIEM request to comply with existing state interfaces or may use other methods to get the data from the State PDMP systems. All of these interactions are isolated from the PDMP Requestor. The Intermediaries may also retrieve data from multiple State PDMP systems simultaneously.
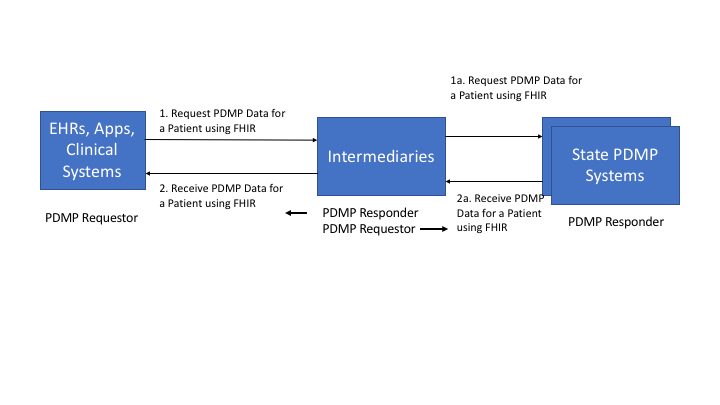
In this deployment option, the EHRs, Apps and Clinical Systems act as the PDMP Requestors and interact with Intermediary Gateways such as Appriss, RxCheck which act as the PDMP Responders. The communication is performed using FHIR APIs. In this case the PDMP Requestors are isolated from the State PDMP Systems and the protocols they support.
The Intermediaries in this case will use FHIR APIs to request data from one or more State PDMP Systems. The advantage here it is the same standard end to end however an Intermediary can provide value added information such as analytics, ability to integrate data from multiple states.
The Intermediary plays the role of PDMP Responder for Transactions 1 and 2 but plays the role of PDMP Requestor for Transactions 1a and 1b where the State PDMP Systems play the PDMP Responder role.
In this deployment option, the EHRs, Apps and Clinical Systems act as the PDMP Requestors and interact with the State PDMP Systems which act as the PDMP Responders using the FHIR APIs
There are no intermediaries being used in this deployment and State PDMP Systems have to support the necessary FHIR APIs and SMART Backend Authorization protocols.