This page is part of the US-Medication FHIR IG (v1.2.0: STU 2) based on FHIR R3. This is the current published version. For a full list of available versions, see the Directory of published versions 
US Meds Prescription Drug Monitoring Program (PDMP) FHIR Implementation Guide
- Introduction
- Scope
- Abstract Model, Actors and Definitions
- EHR - PDMP Data Access Current State
- EHR - PDMP Data Access Using FHIR APIs
- PDMP Data Elements and Mappings
- Capability Statements
- Patient Matching Considerations
- Deployment Architecture
Introduction
In the United States, every state is deploying a Prescription Drug Monitoring Program (PDMP) which track controlled substance prescriptions within the state. Overtime, these PDMP databases start to provide rich information on provider and patient behaviors with respect to prescribing and use of controlled substances (primarily opioids). Enabling a Provider to access a Patient’s PDMP data during care delivery will help avoid potential drug misuse, abuse and diversion. In order to reduce opioid abuse, some states have implemented policies mandating Providers to check the state PDMP for the Patient’s controlled substance history before prescribing controlled substances. To further address opioid abuse which is a current national priority, the US Meds Prescription Drug Monitoring Program FHIR Implementation Guide (US Meds PDMP FHIR IG) outlines how systems can access PDMP data for a patient from the state PDMP systems using the HL7 FHIR standard. For general background on state PDMPs, see the Centers for Disease Control and Prevention what states need to know about PDMPs.
Scope
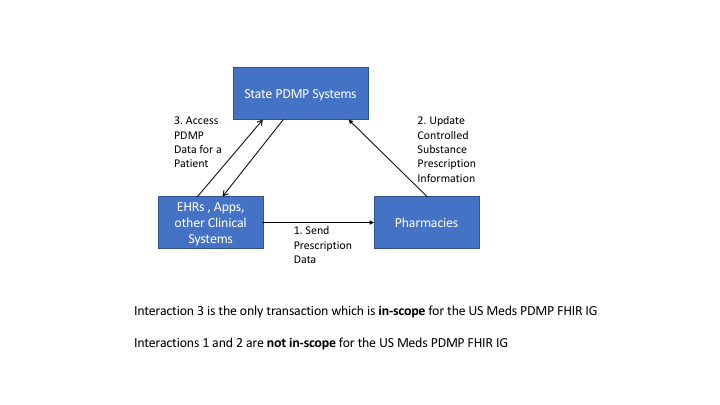
This section outlines the transactions which are in-scope and not in-scope for the US Medications PRMP FHIR Implementation Guide. As shown in the Figure 1 below, the PDMP eco-system can be simplified for the purpose of this project to consist of EHRs or Clinical Systems, Pharmacies and the State PDMP systems.
The US Meds PDMP FHIR IG defines how an EHR or an App or other Clinical Systems can access a Patient’s controlled substance prescription history from the State PDMP systems. This is identified by Interaction 3 in the diagram. All other interactions such as Interaction 1 and 2 in the diagram below are important for the overall PDMP eco-system, they are not in-scope for this project and IG.
Abstract Model, Actors and Definitions
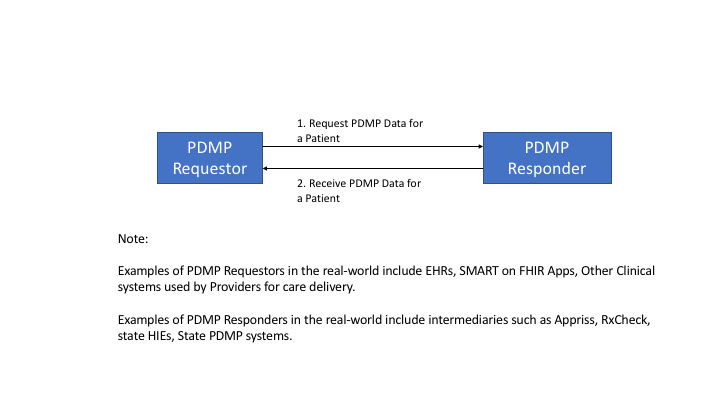
This section defines the abstract model which is used to identify the specific actors and interactions that are in-scope for the project. The abstract model is as shown in Figure 2 below which consists of two actors namely the PDMP Requestor and the PDMP Responder.
PDMP Requestor: PDMP Requestor is a health IT system that is requesting a Patient’s controlled substance history. Real-world examples of such health IT systems include EHRs, SMART on FHIR Apps and other Clinical Systems used for care delivery.
PDMP Responder: PDMP Responder is a health IT system that accepts a request from a PDMP Requestor and responds to the request with a controlled substance history for the patient. Real-world examples of such health IT systems include intermediary gateways such as Appriss, RxCheck, State HIEs and State PDMP systems.
Note: PDMP Responders, which act as intermediaries, provide additional services such as being able to query multiple State PDMP systems for analytics which generates additional information for the Provider. The fact that a PDMP Responder is an intermediary or if it is the actual State PDMP system is transparent to the PDMP Requestor and is more of a deployment architecture.
EHR - PDMP Data Access Current State
In the current PDMP eco-system, EHR systems use a combination of NCPDP SCRIPT and PMIX/NIEM to access data from the state PDMP systems. Figure 3 below shows these data access patterns with and without intermediaries.

As shown in the figure above, a Practitioner uses the EHR to access PDMP data, which then initiates a NCPDP based RxHistoryRequest transaction requesting data for a patient. The request is normally routed to an intermediary such as Appriss, RxCheck or a State Health Information Exchange (HIE) system. The intermediary typically converts this incoming NCPDP request to PMIX/NIEM format and initiates a request to the State PDMP systems. The response then comes back from the State PDMP system in PMIX/NIEM format which the intermediary converts it back to NCPDP RxHistoryResponse and makes it available to the EHR where the Practitioner can view the results.
Another mechanism that is currently used by Practitioners to access PDMP data is by using web portals which is shown in Figure 4 below.
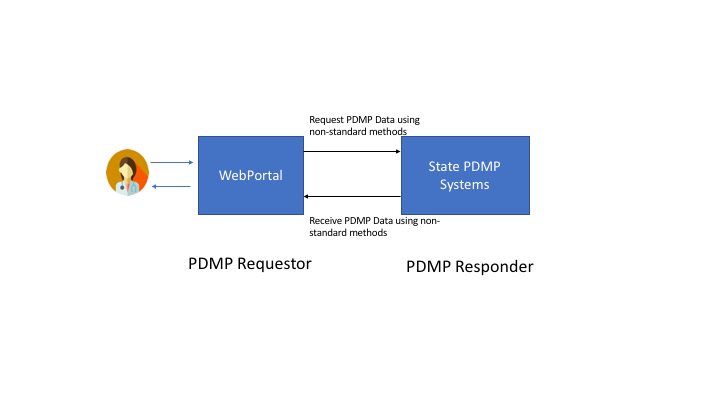
In this case, the Practitioner has to interact with a separate web portal not integrated with the EHR and access the PDMP data. The web portals typically have custom integrations with the State PDMP systems and provide access to data.
EHR - PDMP Data Access Using FHIR APIs
As discussed above, the current mechanisms to access PDMP data vary between the usage of multiple standards namely NCPDP, PMIX/NIEM and usage of proprietary mechanisms such as the web portals. The PDMP eco-system can benefit from the usage of FHIR APIs for accessing PDMP data in the following ways
- Ability to easily integrate PDMP data access in EHR work flows using SMART on FHIR Apps
- Ability to enhance security mechanisms outlined by FHIR and SMART on FHIR between the PDMP actors
- Ability to leverage the PDMP FHIR APIs to build decision support services using CDS Hooks in the EHR work flows
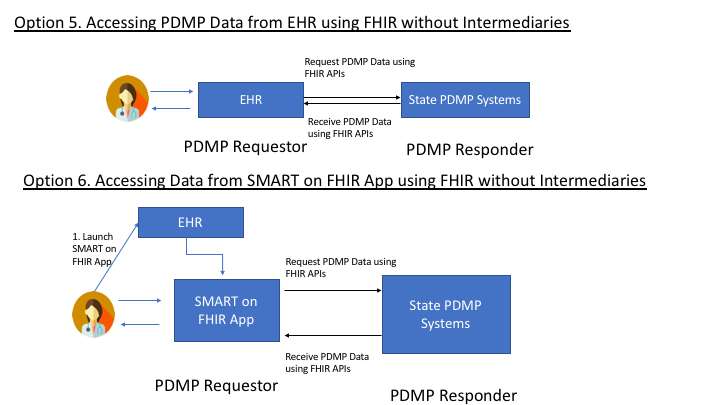
Figure 5a, 5b and 5c below shows the different options for using FHIR APIs to access PDMP data in the EHR work flows including ability to leverage existing investments in intermediaries and PMIX/NIEM protocols.


Profiles to be used
In order to use FHIR to access PDMP data the following FHIR profiles will be used
- MedicationDispense profile: Used to communicate dispense information.
- MedicationRequest profile: Used to communicate prescription information.
- Medication profile: Used to communicate actual drug information.
- Organization profile: Used to communicate information about the dispensing organization.
- Practitioner profile: Used to communicate information about the prescriber.
- Patient profile: Used to communicate information about the patient.
- Message Header: Used to communicate information about the request headers.
API
The FHIR standard provides a rich set of search mechanisms by which specific FHIR resources can be accessed from a FHIR server. Typically the search parameters are specified in the RESTful URL and accessed using the HTTP GET operation.
The following is the exact API that uses multiple search parameters to access PDMP data from a PDMP Responder
`GET [base]/MedicationDispense?subject:Patient.name.given=sherlock&subject:Patient.name.family=holmes&subject:Patient.birthdate=eq1954-01-06&authorizingPrescription.dispenseRequest.validityPeriod=ge1954-01-06&authorizingPrescription.dispenseRequest.validityPeriod=le2019-12-01&_include=MedicationDispense:subject&_include:recurse=MedicationDispense:authorizingPrescription&_include=MedicationDispense:medication`
The above API will fetch all MedicationDispense resources for Patient with a given name of “sherlock” and family name of “holmes” with a birthdate of “1954-01-06” with a prescription from January 6, 1954 to December 01, 2019. The bundle returned will include MedicationDispense, MedicationRequest, Practitioner, Organization, Patient and Medication.
The security considerations for using the API will be discussed as part of the security section.
The data elements that will be returned and how they map to NCPDP and PMIX/NIEM will be discussed in the PDMP Data Elements and Mapping section.
Security Considerations for PDMP Transactions
All implementers of FHIR servers and clients should pay attention to FHIR Security considerations.
In addition to the above, the PDMP transactions between the PDMP Requestor and the PDMP Responder need to be secured using the SMART Backend Services Authorization Guide as shown in Figure 6 below.

PDMP Responder Requirements
- Specifically the PDMP Responder will implement the Authorization Server (documented as EHR Authz Server in the SMART on FHIR Backend Services specification) that will permit the PDMP Requestor to ask for PDMP data about specific patients.
- The PDMP Responder’s Authorization Server will register each PDMP Requestor and provide the capability to register its public key with the Authorization Server.
- The PDMP Responder is expected to allow registration of a PDMP Requestor for each individual Provider or a Provider Organization as required by policies.
- The PDMP Responder SHALL collect the following information about each PDMP Rqquestor which will be used for both auditing and for identifying the requestor uniquely. ** Requestor Identity namely name ** Requestor Role ** Requestor DEA, NPI Number ** Requestor Facility information
PDMP Requestor Requirements
- The PDMP Requestor will implement the requirements corresponding to the App actor in the SMART on FHIR Backend Services specification.
- The PDMP Requestor is expected to run in a trusted environment and hence capable of protecting the Private Key.
Security Considerations for SMART on FHIR App
For deployments using a SMART on FHIR App which plays the role of a PDMP Requestor, the app will be launched from the EHR and secured using the SMART App Launch Framework. The user authorizing the app in this case would be the Practitioner who has access to data about his/her patients.
PDMP Data Elements and Mappings
This section describes and identifies data elements that are used commonly in the PDMP data requests and responses and provides mappings of these data elements to FHIR. Based on environmental scans and prior performed by ONC across a spectrum of PDMP implementations the following data was collected:
- Most of the existing EHR implementations use NCPDP script 10.6 or ASAP web services to request and receive PDMP data from PDMP Responders (Intermediaries or State PDMP systems).
- Most of the State PDMP systems are implemented using data elements specified by the NIEM standard and expose these data elements using PMIX APIs.
- Most of the EHRs use intermediaries to request data from one or more State PDMP systems and send NCPDP based requests and receive responses in NCPDP format.
Based on the above findings, NCPDP Request and Response data elements have been used as a starting point to specify the FHIR APIs. Since the community understands these NCPDP data elements, a mapping of NCPDP Request and Response data elements to FHIR Resources has been created and specified below. This allows organizations already familiar with NCPDP to use the mapping provided to develop their FHIR Resources and APIs. Similarly mapping from PMIX/NIEM data elements to FHIR is also provided for systems using PMIX/NIEM to map their data to FHIR and expose them through appropriate APIs.
NCPDP Mappings for PDMP Request
This section includes the minimal mapping for the PDMP request from an EHR to a state PDMP using NCPDP.
| PDMP Request Data Element | NCPDP Data Element | FHIR Data Element | |
| Routing Information | |||
| Request | Requestor | <Last Name> <First Name> | Practitioner.name |
| Requestor Role | <Qualifer> | PractitionerRole.code | |
| Request ID | <MessageID> | MessageHeader.id | |
| Request date/ timestamp | <SentTime> | MessageHeader.timestamp | |
| Requestor Identifier | NPI Number* | <NPI> | Practitioner.identifier |
| DEA Number* | <DEANumber> | Practitioner.identifier | |
| Requesting Facility ID | DEA Number* | <DEANumber> | Organization.identifier |
| NCPDP Number* | <NCPDPID> | Organization.identifier | |
| NPI* | <NPI> | Organization.identifier | |
| Requesting Faciltiy | Facility Name | <Store Name> <Clinic Name> | Organization.name |
| State code of Requesting Facility | <RequestingState> | Organization.address.state | |
| Message Body | |||
| Patient | First Name | <FirstName> | MedicationDispense.subject(Patient) --> Patient.name.given |
| Last Name | <LastName> | MedicationDispense.subject(Patient) --> Patient.name.family | |
| Date of Birth | <DateofBirth> | MedicationDispense.subject(Patient) --> Patient.birthdate | |
| Request Prescription Date Range | Start Date | <EffectiveDate> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod |
| End Date | <ExpirationDate> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod | |
| * Conditionally required data elements have asterisks (*), meaning at least one data element is required within this category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) is required. | |||
NCPDP Mappings for PDMP Response
This section includes the minimal mapping for the PDMP response from a state PDMP to an EHR using NCPDP.
| PDMP Response Data Element | NCPDP Data Element | FHIR Data Element | |
| Routing Information | |||
| Response Date/Timestamp | <SentTime> | MessageHeader.timestamp | |
| Response Prescription Date Range (Start Date) | <EffectiveDate> | medicationdispense-validityPeriod (Existing MedicationDispense Extension) | |
| Response Prescription Date Range (End date) | <ExpirationDate> | medicationdispense-validityPeriod (Existing MedicationDispense Extension) | |
| Request ID | <RelatesToMessageID> | MessageHeader.response.identifier | |
| Message Body | |||
| Patient | Patient First Name | <FirstName> | Patient.name.given |
| Patient Last Name | <LastName> | Patient.name.family | |
| Patient Date of Birth | <DateOfBirth> | Patient.birthdate | |
| Patient Gender | <Gender> | Patient.gender | |
| Patient Street Address | <AddressLine> <AddressLine2> | Patient.address.line | |
| Patient City Address | <City> | Patient.address.city | |
| Patient State Code | <State> | Patient.address.state | |
| Patient Zip Code | <ZipCode> | Patient.address.postalCode | |
| Patient Identifier | SSN* | <SocialSecurity> | Patient.identifier |
| Prescription | Prescription Filled Date | <LastFillDate> | MedicationDispense.whenPrepared |
| Prescription Written Date | <WrittenDate> | MedicationDispense.authorizingPrescription.authoredOn | |
| Prescription Number | <SourceReference> | MedicationDispense.Identifier | |
| Drug Name[1] | <DrugDescription> | MedicationDispense.medicationReference.code.coding.code.dispay | |
| Drug Strength[1] | <StrengthValue, StrengthUnitOfMeasure> fields | MedicationDispense.medicationReference.ingredient.amount | |
| Dosage Form[2] | <FormCode> | MedicationDispense.medicationReference.form | |
| Drug Quantity | <Quantity> | MedicationDispense.quantity | |
| Days of Supply | <DaysSupply> | MedicationDispense.daysSupply | |
| Refill Number | <FillNumber> | MedicationDispense.extension - (Proposed new extension - fillNumber) | |
| Refills Authorized | <Refills> | MedicationDispense.authorizingPrescription.dispenseRequest.numberOfRepeatsAllowed | |
| Partial Fill Indicator | <FillStatus> | MedicationDispense.type | |
| Method of Payment | <Note> | MedicationDispense.note | |
| Drug | Product ID Qualifier | <CodeListQualifier> | MedicationDipense.medicationReference.code.coding.system |
| Product ID | <ProductCode> | MedicationDispense.medicationReference.code.coding.code | |
| Dispenser Organization | Dispenser Organization Name (Facility) | <StoreName> | Organization.name |
| Dispenser Organization Street Address | <AddressLine> <AddressLine2> | Organization.address.line | |
| Dispenser Organization City Address | <City> | Organization.address.city | |
| Dispenser Organization State Code | <State> | Organization.address.state | |
| Dispenser Organization Zip Code | <ZipCode> | Organization.address.postalCode | |
| Dispenser Organization Phone Number | <CommunicationNumber> | Organization.telecom | |
| Dispenser Organization (Pharmacy identifier) | DEA Number* | <DEANumber> | Organization.identifier |
| NCPDP Number* | <NCPDPID> | Organization.identifier | |
| NPI Number* | <NPI> | Organization.identifier | |
| Prescriber | Prescriber First Name | <FirstName> | Practitioner.name.given |
| Prescriber Last Name | <LastName> | Practitioner.name.family | |
| Prescriber Street Address | <AddressLine> <AddressLine2> | Practitioner.address.line | |
| Prescriber City Address | <City> | Practitioner.address.city | |
| Prescriber State Code | <State> | Practitioner.address.state | |
| Prescriber Zip Code | <ZipCode> | Practitioner.address.postalCode | |
| Prescriber Identifier | DEA Number* | <DEANumber> | Practitioner.identifier |
| NPI Number* | <NPI> | Practitioner.identifier | |
| State License* Identifier | NA | Practitioner.identifier | |
| State of License* | NA | Practitioner.identifier | |
| * Conditionally required data elements have asterisks (*), meaning at least one data element is required within this category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) is required. Similarly for Patient Identifier, either SSN or MedicareNumber should be used as allowed by law. Additional occurrences of Patient Identifier may use PatientAccountNumber of MedicalRecordIdentificationNumberEHR per the NCPDP Script implementation guide. | |||
PMIX Mappings for PDMP Request
This section includes the minimal mapping for the PDMP request from an EHR to a state PDMP using PMIX.
| PDMP Request Data Element | PMIX Data Element | FHIR Data Element | |
| Routing Information | |||
| Request | Requestor | <pmix:Requestor> | Practitioner.name |
| Requestor Role | <pmix:RequestorRole> | PractitionerRole.code | |
| Request ID | <pmix:RequestID> | MessageHeader.id | |
| Request date/ timestamp | n/a | MessageHeader.timestamp | |
| Requestor Identifier | NPI Number* | <nc:IdentificationID> | Practitioner.identifier |
| DEA Number* | <nc:IdentificationID> | Practitioner.identifier | |
| Requesting Facility ID | DEA Number* | <nc:IdentificationID> | Organization.identifier |
| NCPDP Number* | <nc:IdentificationID> | Organization.identifier | |
| NPI* | <nc:IdentificationID> | Organization.identifier | |
| Requesting Faciltiy | Facility Name | <nc:OrganizationDoingBusinessAsName> | Organization.name |
| State code of Requesting Facility | <nc:LocationStateUSPostalServiceCode> | Organization.address.state | |
| Message Body | |||
| Patient | First Name | <nc:PersonGivenName> | MedicationDispense.subject(Patient) --> Patient.name.given |
| Last Name | <nc:PersonSurName> | MedicationDispense.subject(Patient) --> Patient.name.family | |
| Date of Birth | <nc:Date> | MedicationDispense.subject(Patient) --> Patient.birthdate | |
| Request Prescription Date Range | Start Date | <pmp:RequestPrescriptionDateRangeBegin> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod |
| End Date | <pmp:RequestPrescriptionDateRangeEnd> | MedicationDispense.authorizingPrescription.dispenseRequest.validityPeriod | |
| * Conditionally required data elements have asterisks (*), meaning at least one data element is required within this category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) is required. | |||
PMIX Mappings for PDMP Response
This section includes the minimal mapping for the PDMP response from a state PDMP to an EHR using PMIX.
| PDMP Response Data Element | PMIX Data Element | FHIR Data Element | |
| Routing Information | |||
| Response Date/Timestamp | <pmp:ReportExecutionDate><pmp:ReportExecutionTime> | MessageHeader.timestamp | |
| Response Prescription Date Range (Start Date) | <pmp:ReportDateRangeBegin> | medicationdispense-validityPeriod (Existing MedicationDispense Extension) | |
| Response Prescription Date Range (End date) | <pmp:ReportDateRangeEnd> | medicationdispense-validityPeriod (Existing MedicationDispense Extension) | |
| Request ID | n/a | MessageHeader.response.identifier | |
| Message Body | |||
| Patient | Patient First Name | <nc:PersonGivenName> | Patient.name.given |
| Patient Last Name | <nc:PersonSurName> | Patient.name.family | |
| Patient Date of Birth | <nc:Date> | Patient.birthdate | |
| Patient Gender | <PersonSexCode> | Patient.gender | |
| Patient Street Address | <StreetFullText> | Patient.address.line | |
| Patient City Address | <nc:LocationCityName> | Patient.address.city | |
| Patient State Code | <nc:LocationStateUSPostalServiceCode> | Patient.address.state | |
| Patient Zip Code | <nc:LocationPostalExtensionCod> | Patient.address.postalCode | |
| Patient Identifier | SSN* | <nc:IdentificationID> | Patient.identifier |
| Prescription | Prescription Filled Date | <pmp:ReportDateRangeBegin><pmp:ReportDateRangeEnd> | MedicationDispense.whenPrepared |
| Prescription Written Date | <nc:Date> | MedicationDispense.authorizingPrescription.authoredOn | |
| Prescription Number | <pmp:PrescriptionNumberText> | MedicationDispense.Identifier | |
| Drug Name[1] | <pmp:DrugProductNameText> | MedicationDispense.medicationReference.code.coding.code.dispay | |
| Drug Strength[1] | <pmp:DrugStrengthText> | MedicationDispense.medicationReference.ingredient.amount | |
| Dosage Form[2] | <pmp:DrugUnitOfMeasureText> | MedicationDispense.medicationReference.form | |
| Drug Quantity | <pmp:DispensedQuantity> | MedicationDispense.quantity | |
| Days of Supply | <pmp:DaysSupplyCount> | MedicationDispense.daysSupply | |
| Refill Number | <pmp:DrugRefillNumberCount> | MedicationDispense.extension - (Proposed new extension - fillNumber) | |
| Refills Authorized | <pmp:RefillsAuthorizedCount> | MedicationDispense.authorizingPrescription.dispenseRequest.numberOfRepeatsAllowed | |
| Partial Fill Indicator | <pmp:PartialFillIndicator> | MedicationDispense.type | |
| Method of Payment | <pmp:MethodOfPaymentCode> | MedicationDispense.note | |
| Drug | Product ID Qualifier | <pmp:DrugCPDProductIdentifier><pmp:DrugDINProductIdentifier></br><pmp:DrugHRIProductIdentifier><pmp:pmp:DrugNDCProductIdentifier></br><pmp:DrugUPCProductIdentifie><pmp:DrugUPNProductIdentifier> | MedicationDipense.medicationReference.code.coding.system |
| Product ID | <IdentificationID> | MedicationDipense.medicationReference.code.coding.code | |
| Dispenser Organization | Dispenser Organization Name (Facility) | <nc:OrganizationDoingBusinessAsName> | Organization.name |
| Dispenser Organization Street Address | <nc:StreetFullText> | Organization.address.line | |
| Dispenser Organization City Address | <nc:LocationCityName> | Organization.address.city | |
| Dispenser Organization State Code | <nc:LocationStateUSPostalServiceCode> | Organization.address.state | |
| Dispenser Organization Zip Code | <nc:LocationPostalCode> | Organization.address.postalCode | |
| Dispenser Organization Phone Number | <nc:TelephoneNumberFullID> | Organization.telecom | |
| Dispenser Organization (Pharmacy identifier) | DEA Number* | <nc:IdentificationIDgt; | Organization.identifier |
| NCPDP Number* | <nc:IdentificationID> | Organization.identifier | |
| NPI Number* | <nc:IdentificationID> | Organization.identifier | |
| Prescriber | Prescriber First Name | <nc:PersonGivenName> | Practitioner.name.given |
| Prescriber Last Name | <nc:PersonSurName> | Practitioner.name.family | |
| Prescriber Street Address | <nc:StreetFullText> | Practitioner.address.line | |
| Prescriber City Address | <nc:LocationCityName> | Practitioner.address.city | |
| Prescriber State Code | <nc:LocationStateUSPostalServiceCode> | Practitioner.address.state | |
| Prescriber Zip Code | <LocationPostalCode> | Practitioner.address.postalCode | |
| Prescriber Identifier | DEA Number* | <IdentificationID> | Practitioner.identifier |
| NPI Number* | <IdentificationID> | Practitioner.identifier | |
| State License* Identifier | IdentificationID | Practitioner.identifier | |
| State of License* | IdentificationID | Practitioner.identifier | |
| * Conditionally required data elements have asterisks (*), meaning at least one data element is required within this category. For example, under Requesting Facility ID, one of the three data elements (DEA Number, NCPDP Number or NPI) is required. Similarly for Patient Identifier, either SSN or MedicareNumber should be used as allowed by law. Additional occurrences of Patient Identifier may use PatientAccountNumber of MedicalRecordIdentificationNumberEHR per the NCPDP Script implementation guide. | |||
FHIR profiles
This project does not create any new profiles, but will reuse the US-Core profiles and the US Meds profiles to request and receive PDMP data using FHIR resources.
Capability Statements
This section identifies the CapabilityStatements defined for this implementation guide. The section outlines conformance requirements for each of the US Meds PDMP FHIR IG actors which includes the specific profiles, operations, security mechanisms and search parameters that need to be supported.
Note: The individual profiles identify the structural constraints, terminology bindings and invariants.
Conformance requirements for the PDMP Responder
The section describes the expected capabilities of the PDMP Responder actor which is responsible for providing responses to the queries submitted by the PDMP Requestor applications.
Behavior
The PDMP Responder SHALL:
- Support the US Core Patient, US Core Practitioner, US Core Organization resource profiles.
- Support the US Meds MedicationRequest and MedicationDispense Profile.
- Implement the RESTful behavior according to the FHIR specification.
- which includes returning the following response classes:
- (Status 200): successful operation
- (Status 400): invalid parameter
- (Status 401/4xx): unauthorized request
- (Status 403): insufficient scope
- (Status 404): unknown resource
- (Status 410): deleted resource.
- which includes returning the following response classes:
- Support json resource formats for all PDMP interactions.
- Declare a CapabilityStatement identifying the list of profiles, operations, and search parameters supported.
The PDMP Responder SHOULD:
- Support the following US Core and US Meds resource profiles:
- US Core Medication
- US Meds MedicationAdministration
- Support xml resource formats for all US Meds interactions.
- Identify the US Core profile(s) and US Meds profiles supported as part of the FHIR meta.profile attribute for each instance.
The PDMP Responder MAY:
- Support other US Core and US Meds resource profile
Profile Interactions:
-
The PDMP Responder SHALL support the FHIR Search interaction for MedicationDispense profile.
-
The PDMP Responder SHOULD support the FHIR Read profile interaction MedicationDispense profile.
-
The PDMP Responder MAY support other FHIR profile interactions.
Security:
-
The PDMP Responder SHALL support the SMART Backend Services Authorization Guide for verifying authentication and providing authorization to PDMP Requestors.
-
The PDMP Responder SHALL support the HTTP Header parameter X-Request-ID for request coorelation between the PDMP Requester and PDMP Responder.
Search:
The PDMP Responder SHALL support the following search parameters and combination for the MedicationDispense resource
- Chained Search parameters
- subject:Patient.name.given - Patient’s first name
- subject:Patient.name.family - Patient’s family name
- subject:Patient.birthdate - Patient’s birth date
- authorizingPrescription.dispenseRequest.validityPeriod - To specify the date range for the PDMP data retrieval
The PDMP Responder SHALL support the following _include parameters for the MedicationDispense Search operations
- _include=MedicationDispense:subject - Returns the Patient Resource information
- _include:recurse=MedicationDispense:authorizingPrescription - Returns the MedicationRequest, Practitioner Resource information and Organization information
- _include=MedicationDispense:medication - Returns the Medication Resource information
The following is an example of the query.
GET [base]/MedicationDispense?subject:Patient.name.given=peter&subject:Patient.name.family=jacobs&subject:Patient.birthdate=eq1973-11-25&authorizingPrescription.dispenseRequest.validityPeriod=ge2010-01-01&authorizingPrescription.dispenseRequest.validityPeriod=le2015-12-31&_include=MedicationDispense:subject&_include:recurse=MedicationDispense:authorizingPrescription&_include=MedicationDispense:medication
The above API will fetch all MedicationDispense resources for Patient with a given name of “peter” and family name of “jacobs” with a birthdate of “1973-11-25” with a prescription that falls within in a 5 year window starting from January 1st 2010 to December 31st 2015 and as part of the returned information will include MedicationDispense, MedicationRequest, Practitioner, Organization, Patient and Medication information as part of the returned bundle.
All other information required to authenticate and authorize a PDMP Requestor is captured as part of registering the PDMP Requestor following the SMART Backend Services Authorization Guide.
Conformance requirements for the PDMP Requestor
The section describes the expected capabilities of the PDMP Requestor actor which is responsible for providing responses to the queries submitted by the PDMP Requestor applications.
Behavior
The PDMP Requestor SHALL:
- Support the US Core Patient, US Core Practitioner, US Core Organization resource profiles.
- Support the US Meds MedicationRequest and MedicationDispense Profile.
- Consume the RESTful responses according to the FHIR specification.
- which includes returning the following response classes:
- (Status 200): successful operation
- (Status 400): invalid parameter
- (Status 401/4xx): unauthorized request
- (Status 403): insufficient scope
- (Status 404): unknown resource
- (Status 410): deleted resource.
- which includes returning the following response classes:
- Support json resource formats for all PDMP interactions.
The PDMP Requestor SHOULD:
- Support the following US Core and US Meds resource profiles:
- US Core Medication
- US Meds MedicationAdministration
- Support xml resource formats for all PDMP interactions.
Profile Interactions:
-
The PDMP Requestor SHALL support the FHIR Search interaction for MedicationDispense profile.
-
The PDMP Requestor SHOULD support the FHIR Read profile interaction for MedicationDispense profile.
-
The PDMP Requestor MAY support other FHIR profile interactions.
Security:
-
The PDMP Requestor SHALL support the SMART Backend Services Authorization Guide applicable to clients.
-
The PDMP Requestor SHALL add the HTTP Header parameter X-Request-ID as part of the Search request for request coorelation between the PDMP Requester and PDMP Responder.
Search:
The PDMP Requestor SHALL invoke the Search operation on the PDMP Responder including the following search and _include parameters when requesting PDMP data using the MedicationDispense resource
- Chained Search parameters
- subject:Patient.name.given - Patient’s first name
- subject:Patient.name.family - Patient’s family name
- subject:Patient.birthdate - Patient’s birth date
- authorizingPrescription.dispenseRequest.validityPeriod - To specify the date range for the PDMP data retrieval
The PDMP Requestor SHALL include the following _include parameters for the MedicationDispense Search operations
- _include=MedicationDispense:subject - Returns the Patient Resource information
- _include:recurse=MedicationDispense:authorizingPrescription - Returns the MedicationRequest, Practitioner Resource information and Organization information
- _include=MedicationDispense:medication - Returns the Medication Resource information
The following is an example of the query.
GET [base]/MedicationDispense?subject:Patient.name.given=peter&subject:Patient.name.family=jacobs&subject:Patient.birthdate=eq1973-11-25&authorizingPrescription.dispenseRequest.validityPeriod=ge2010-01-01&authorizingPrescription.dispenseRequest.validityPeriod=le2015-12-31&_include=MedicationDispense:subject&_include:recurse=MedicationDispense:authorizingPrescription&_include=MedicationDispense:medication
The above API will fetch all MedicationDispense resources for Patient with a given name of “peter” and family name of “jacobs” with a birthdate of “1973-11-25” with a prescription that falls within in a 5 year window starting from January 1st 2010 to December 31st 2015 and as part of the returned information will include MedicationDispense, MedicationRequest, Practitioner, Organization, Patient and Medication information as part of the returned bundle.
Patient Matching Considerations
The US Meds PDMP FHIR IG does not add any patient matching requirements to the PDMP actors, but relies on existing practices used for patient matching based on the first name, last name and date of birth provided through the request. Some states may require requesters to include additional parameters to facilitate more accurate patient matching results, however these variations are out of scope for this IG.
Deployment Architecture
The following are deployment options showing how the US Meds PDMP FHIR IG can be used to implement the various actors.
Deployment Option 1:
In this deployment option, the EHRs, Apps and Clinical Systems act as the PDMP Requestors and interact with Intermediary Gateways such as Appriss, RxCheck which act as the PDMP Responders. The communication is performed using FHIR APIs. In this case the PDMP Requestors are isolated from the State PDMP Systems and the protocols they support.
The Intermediaries may translate the incoming FHIR request for data to a PMIX/NIEM request to comply with existing state interfaces or may use other methods to get the data from the State PDMP systems. All of these interactions are isolated from the PDMP Requestor. The Intermediaries may also retrieve data from multiple State PDMP systems simultaneously.

Deployment Option 2:
In this deployment option, the EHRs, Apps and Clinical Systems act as the PDMP Requestors and interact with Intermediary Gateways such as Appriss, RxCheck which act as the PDMP Responders. The communication is performed using FHIR APIs. In this case the PDMP Requestors are isolated from the State PDMP Systems and the protocols they support.
The Intermediaries in this case will use FHIR APIs to request data from one or more State PDMP Systems. The advantage here it is the same standard end to end however an Intermediary can provide value added information such as analytics, ability to integrate data from multiple states.
The Intermediary plays the role of PDMP Responder for Transactions 1 and 2 but plays the role of PDMP Requestor for Transactions 1a and 1b where the State PDMP Systems play the PDMP Responder role.

Deployment Option 3:
In this deployment option, the EHRs, Apps and Clinical Systems act as the PDMP Requestors and interact with the State PDMP Systems which act as the PDMP Responders using the FHIR APIs
There are no intermediaries being used in this deployment and State PDMP Systems have to support the necessary FHIR APIs and SMART Backend Authorization protocols.




