This page is part of the PACIO Advance Directive Information Implementation Guide (v1.0.0: STU 1) based on FHIR (HL7® FHIR® Standard) R4. This is the current published version in its permanent home (it will always be available at this URL). For a full list of available versions, see the Directory of published versions
This section provides additional guidance on the relationship between the associated profiles and the structure of the interoperable advance directive document.
There is a very important distinction for the three types of ADI content that will be covered in this IG. Below is a description of each type of content that will be covered by the ADI FHIR IG with versions.
Type I: Person-Authored Advance Directive Information |
||
|---|---|---|
|
||
Type II: Encounter-Centric Instructions |
||
|
||
Type III: Portable Medical Orders for Life-Sustaining Treatments |
||
|
||
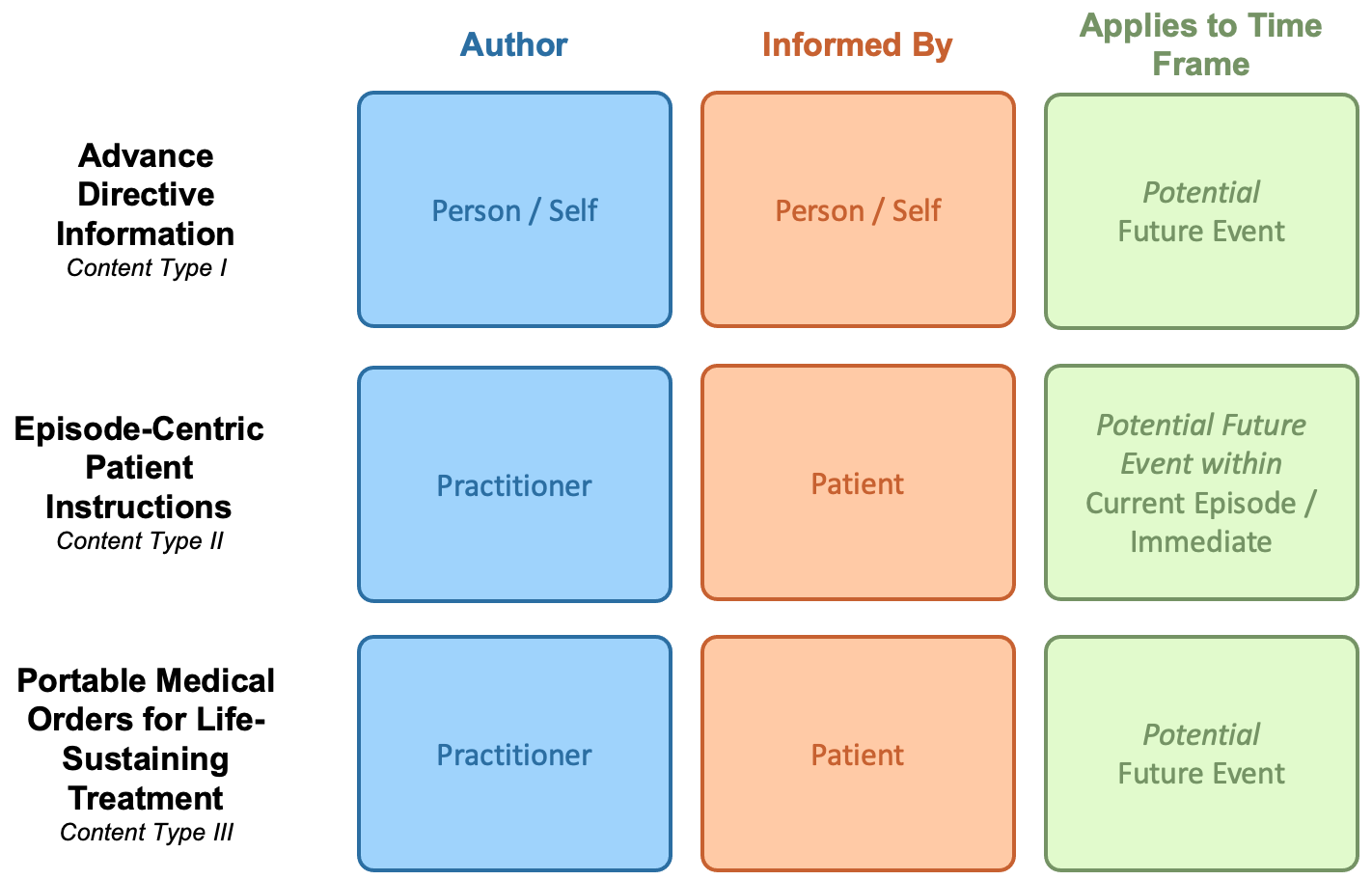
The current version, STU1, of this ADI with FHIR IG covers the use of RESTful API interactions for creation, sharing, query/access, and verification of advance directive information between systems. It is intended to address advance directive interoperability needs for Content Type 1, where the author is the individual that is making medical intervention goals, preferences, priorities known in advance. This IG is not intended to cover medical intervention goals, preferences, priorities for individuals who are not able to create and document their own advance healthcare decisions.
STU1 supports only Person-authored Advance Directives (ADI Content Type 1) documents. Future versions of this FHIR IG will address encounter-centric patient instructions, Content Type 2, and portable medical orders for life-sustaining treatment, Content Type 3.
Advance healthcare decision documents may take several forms, including scanned PDF documents, CDA documents, other binary documents, as well as native FHIR documents (using the Composition and other ADI-specific profiled FHIR resources). This guide defines the interoperable guidance necessary to support creation, update, query, and access to all of these types and other potential ADI document types (through encoding in a Binary resource). Today, most of these documents are shared through scanned images housed in EMRs, EHRs and other systems.
This implementation guide is designed to guide a range of digitization levels, ranging from scanned documents to fully discrete FHIR documents. Additionally, this guide provides the capability for different types of ADI data to be more interoperably digitized than others inside the same document, which is structured as a FHIR Composition, and is described in more detail in the ADI FHIR Document Structure section.
The DocumentReference is the resource that is used for “indexing” of documents, similar to the way a library uses a card catalog to index books based on different search criteria, for example, by title, author, date, or classification code. The DocumentReference can be used in the same way for searching and finding documents with specific attributes such as type of document, subject (e.g., patient), author, dates. These attributes are provided in the metadata of the DocumentReference so that the actual documents do not have to be accessed for most common searches. A complete list of search capabilities on DocumentReference can be found in the Search Parameters section.
Digital signatures are defined as optional in this guide, for a myriad of factors including maturity of systems that can create and exchange digital ADI. If supported by a Content Creator system, the digital signature will be a captured in a Binary resource that is referenced by an additional DocumentReference resource.
There is movement within the FHIR community to move towards using the Provenance resource as a standard way to apply a digital signature to a document in FHIR. The signature within the Provenance resource would be used to encrypt the binary (the actual document itself), not the DocumentReference. A future version of the implementation guide will be updated to follow the standard FHIR guidance on signatures when it is finalized.
ADI native documents using FHIR are instances of the Bundle resource with the type = document. The document should have all content contained within the Bundle with no external references except for the references to external documents in the DocumentationObservation through the focus data element. FHIR Bundle documents consist of multiple entry resources within it, with the first entry being a Composition resource. The Composition resource acts as the header and organizational construct. It contains information about the document such as the category of document, dates, and references to the various participants of the document, as well as document sections used to categorize or organize the contained entries.
The ADI Content Type 1 document defines 7 sections:
Click a block to see the corresponding profile definition
The content in these categories of advance directive could include, but are not limited to:
Content type 1 also includes identifying the presence of any type of Portable Medical Order (PMO) such as a POLST or MOLST, and orders such as Do Not Resuscitate (DNR) orders. It also includes identifying other types of person-authored ADI that might exist outside of the document being reviewed. It does not include the specifics of the structured information content of other PMO and/or DNR documents, but instead creates awareness as to the presence of the documents.
Content Type 2, Episode-Centric Patient Instructions, are used when a person is about to undergo a medical procedure during which there is the potential need to deploy life-sustaining treatments. This type of ADI information can also be used when a person is about to have an inpatient stay, or a stay at a nursing or rehab care facility, where the care delivery team asks the individual to make decisions about medical treatments they do or do not want, should circumstances arise when these decisions need to be made and the individual’s choices would need to be taken into consideration. A person may make these decisions for his or her self, and is sometimes the case if the person cannot make these decisions, the healthcare agent may decide. These medical treatment decisions are made in the present and ONLY apply to the current episode of care. They are instructions provided by the person or their surrogate decision-maker. These instructions are closely related to advance directives, in that they say, if x happens, then do y. Or, if x happens, do not do y. For this reason, these kinds of instructions and prohibitions are often recorded with a person’s advance directives. However, they are not advance directives because they represent treatment instructions that ONLY apply to the current episode of care. These instructions are considered obligation or prohibition instructions, provided by the person or their surrogate decision-maker, and authored by a practitioner.
Content Type 3, are Portable Medical Orders (such as a DNR and/or POLST/MOLST orders). These documents tell other healthcare professionals what the treatment intervention preferences are for a person, and are usually intended to be created when there is an expectation of a limited life-expectancy. Portable medical order documents are authored by practitioners, not patients, and are legal physician orders. They do not document goals, preferences, and priorities that a patient intends to be referenced as guidance when making care decisions but instead focus on medical treatment intervention decisions that already have been made so as to guide treatment interventions.
All doctors, emergency medical professionals, and other healthcare professionals, must follow these portable medical orders as the person moves from one location to another (hospital, care facility, home, etc.), unless another practitioner examines the person, reviews the orders with the person or their healthcare agent, and a decision is reached that changes to the orders are warranted or desired. In an emergency situation, life-sustaining procedures that are normally required of emergency response personnel will be overridden by the contents of portable medical orders.
Depending on the state, portable medical orders may be known by any of the following names:
Portable medical orders are not advance directives and should not be confused with them:
These are important distinctions to understand.
Advance directive documents often contain additional information, or clauses, related to specific areas of the document. This may include things like additional observations about which named healthcare agent is to be primary versus back-up, or a healthcare agent has been selected, or a statement by the author of the document that is felt to be important to the overall contents, and other information that provides context to the data otherwise expressed in the sections or entries of an ADI document. To support this information this guide has defined a Clause extension to all of the Composition sections and various profiles and elements.
The table below describes the FHIR profiles relevant to each of the ADI Content Types.
| CONTENT TYPE I: Advance Directive Information (in STU1 scope) | |||
|---|---|---|---|
| Name of Profile to be developed | Short description | Based On | |
| 1 | ADI Document Reference | This profile defines constraints that represent the information needed to register an advance directive information document on a FHIR server. |
US Core DocumentReference |
| 2 | ADI Header | This profile defines constraints that represent common administrative and demographic concepts for advance directives information used in US Realm clinical documents. |
ClinicalDocument |
| 3 | ADI Personal Advance Care Plan Composition | This profile encompasses information that makes up the author’s advance care planning information. |
ADI Header |
| 4 | ADI Participant | This profile represents a person participating in a person's advance directives in some designated capacity such as healthcare agent or healthcare agent advisor. |
RelatedPerson |
| 5 | ADI Participant Consent | This profile is used to represent the author’s consent for an ADI participant such as a healthcare agent or advisor and can include powers granted to, or limitations imposed upon, such persons. |
Consent |
| 6 | ADI Documentation Observation | This profile is used to indicate if additional advance directive documents, such as physician order for life sustaining treatment (MOLST or POLST) or Do Not Resuscitate Order (DNR) exist and a reference to the document. |
Observation |
| 8 | ADI Personal Intervention Preference | This profile is used to represent personal medical intervention preferences under certain health conditions. |
Observation |
| 9 | ADI Care Experience Preference | This profile is used to express the author's personal thoughts about something he or she feels is relevant to his or her care experience which can be important to know when planning or delivering his or her care. |
Observation |
| 10 | ADI Personal Goal | This profile is a statement that presents the author's personal health goals that are important to be mindful of when planning his or her care. |
US Core Goal |
| 11 | ADI Personal Priorities Organizer | This profile is used to represent a set of personal goals, preferences or care experiences in a preferred ranked order. |
List |
| 12 | ADI Organ Donation Observation | This profile is used to represent the author's thoughts about organ donation. |
Observation |
| 13 | ADI Autopsy Observation | This profile is used to represent the author's thoughts about autopsy. |
Observation |
| 13 | ADI Preference Care Plan | The Preference Care Plan is a means for an individual to express their goals and preferences under certain circumstances that may be pertinent when planning his or her care. |
Care Plan |
| 13 | ADI Provenance | Advance Directive Interoperability Provenance based on US Core to capture, search and fetch provenance information associated with advance directive interoperability data. |
US Core Provenance |
| CONTENT TYPE II: Encounter-Centric Patient Instructions (after STU1) | |||
| Name of Profile to be developed | Short description | Based On | |
| 15 | ADI Obligation Instruction | This profile always expresses activities that care providers have been instructed by the person or their healthcare agent to perform. |
Consent |
| 16 | ADI Prohibition Instruction | This profile always expresses activities that care providers have been instructed by the person or their healthcare agent not to perform. |
Consent |
| 17 | Advance Directives Organizer | This profile groups a set of ADI observations documented together at a single point in time and are ONLY relevant during the episode of care being documented. |
List |
| 18 | ADI Advance Directives Observation | This profile is used to record information about ADI authored by the person which contains goals, preferences, and priorities for care. |
Observation |
| 19 | ADI Advance Care Planning Intervention | This profile is used to record a planned intervention that will involve reviewing and verifying a person’s goals, preferences or priorities for treatment or will involve educating and supporting a person on establishing or modifying his or her ADI. |
US Core Procedure |
| CONTENT Type III: P/MOLST (after STU1) | |||
| Name of Profile to be developed | Short description | Based On | |
| 20 | ADI Consent for Portable Medical Orders | This profile is used to express the person, or their healthcare agent’s, consent that is not bound by an encounter. |
Consent |
| 21 | ADI Consent for DNR Orders | This profile is used to express the patient’s or healthcare agent consent that is not bound by an encounter. |
Consent |
| Sharing Documents | |||
| Name of Profile to be developed | Short description | Based On | |
| 22 | ADI Consent to Share | This profile is used to enable someone else to act on their behalf if they are unable to do so themselves. |
Consent |
There are no Global profiles defined
This Implemention Guide is based on FHIR R4.
Package hl7.fhir.us.core#4.0.0 The US Core Implementation Guide is based on FHIR Version R4 and defines the minimum conformance requirements for accessing patient data. The Argonaut pilot implementations, ONC 2015 Edition Common Clinical Data Set (CCDS), and ONC U.S. Core Data for Interoperability (USCDI) v1 provided the requirements for this guide. The prior Argonaut search and vocabulary requirements, based on FHIR DSTU2, are updated in this guide to support FHIR Version R4. This guide was used as the basis for further testing and guidance by the Argonaut Project Team to provide additional content and guidance specific to Data Query Access for purpose of ONC Certification testing. These profiles are the foundation for future US Realm FHIR implementation guides. In addition to Argonaut, they are used by DAF-Research, QI-Core, and CIMI. Under the guidance of HL7 and the HL7 US Realm Steering Committee, the content will expand in future versions to meet the needs specific to the US Realm. These requirements were originally developed, balloted, and published in FHIR DSTU2 as part of the Office of the National Coordinator for Health Information Technology (ONC) sponsored Data Access Framework (DAF) project. For more information on how DAF became US Core see the US Core change notes. (built Mon, Jun 28, 2021 19:09+0000+00:00) |
Package hl7.fhir.uv.extensions#1.0.0 This IG defines the global extensions - the ones defined for everyone. These extensions are always in scope wherever FHIR is being used (built Sun, Mar 26, 2023 08:46+1100+11:00) |
Package hl7.fhir.uv.extensions.r4#1.0.0 This IG defines the global extensions - the ones defined for everyone. These extensions are always in scope wherever FHIR is being used (built Sun, Mar 26, 2023 08:46+1100+11:00) |