This page is part of the Da Vinci Data Exchange for Quality Measures (DEQM) FHIR IG (v1.0.0: STU 1) based on FHIR (HL7® FHIR® Standard) R3. The current version which supersedes this version is 5.0.0. For a full list of available versions, see the Directory of published versions
Venous Thromboembolism Prophylaxis Use Case
Introduction
The VTE-1 measure assesses the number of patients who received venous thromboembolism (VTE) prophylaxis or have documentation why no venous thromboembolism prophylaxis was given the day of or the day after hospital admission or surgery end date for surgeries that start the day of or the day after hospital admission. Note that the Individual Measure Reporting Interaction is the only interaction used for this measure.
The example presented is based on the QDM version of CMS 108v7, which has been represented using profiles derived from QI Core. Additional information regarding the measure specification can be found in the Quality Measure Implementation Guide
FHIR Resource Overview
Resources supported for this Use Case
| Resource Type | Profile Name | Link to Profile |
|---|---|---|
| Condition | QI Core Condition Profile | QI Core Condition |
| Coverage | QI Core Coverage Profile | QI Core Coverage |
| DeviceRequest | DEQM DeviceRequest Profile | DEQM DeviceRequest |
| DeviceUseStatement | DEQM DeviceUseStatement Profile | DEQM DeviceUseStatement |
| Encounter | QI Core Encounter Profile | QI Core Encounter |
| Library | CQFM Library Profile | CQFM Library |
| Location | QI Core Location Profile | QI Core Location |
| Measure | CQFM Measure Profile | CQFM Measure |
| MeasureReport | DEQM Individual MeasureReport Profile | DEQM Individual MeasureReport Profile |
| MeasureReport | DEQM Summary MeasureReport Profile | DEQM Summary MeasureReport Profile |
| MedicationAdministration | DEQM MedicationAdministration Profile | DEQM MedicationAdministration |
| MedicationRequest | DEQM MedicationRequest Profile | DEQM MedicationRequest |
| Observation | QI Core Observation Profile | QI Core Observation |
| Organization | DEQM Organization Profile | DEQM Organization |
| Patient | QI Core Patient Profile | QI Core Patient |
| Practitioner | DEQM Practitioner Profile | DEQM Practitioner |
| Procedure | QI Core Procedure Profile | QI Core Procedure |
| ProcedureRequest | QI Core ProcedureRequest Profile | QI Core ProcedureRequest |
Graph of VTE-1 Resources
In this section we list resource graph diagrams for 7 clinical scenarios that meet the VTE-1 measure. Note that overlapping boxes in the diagrams represents a choice of one the resources.
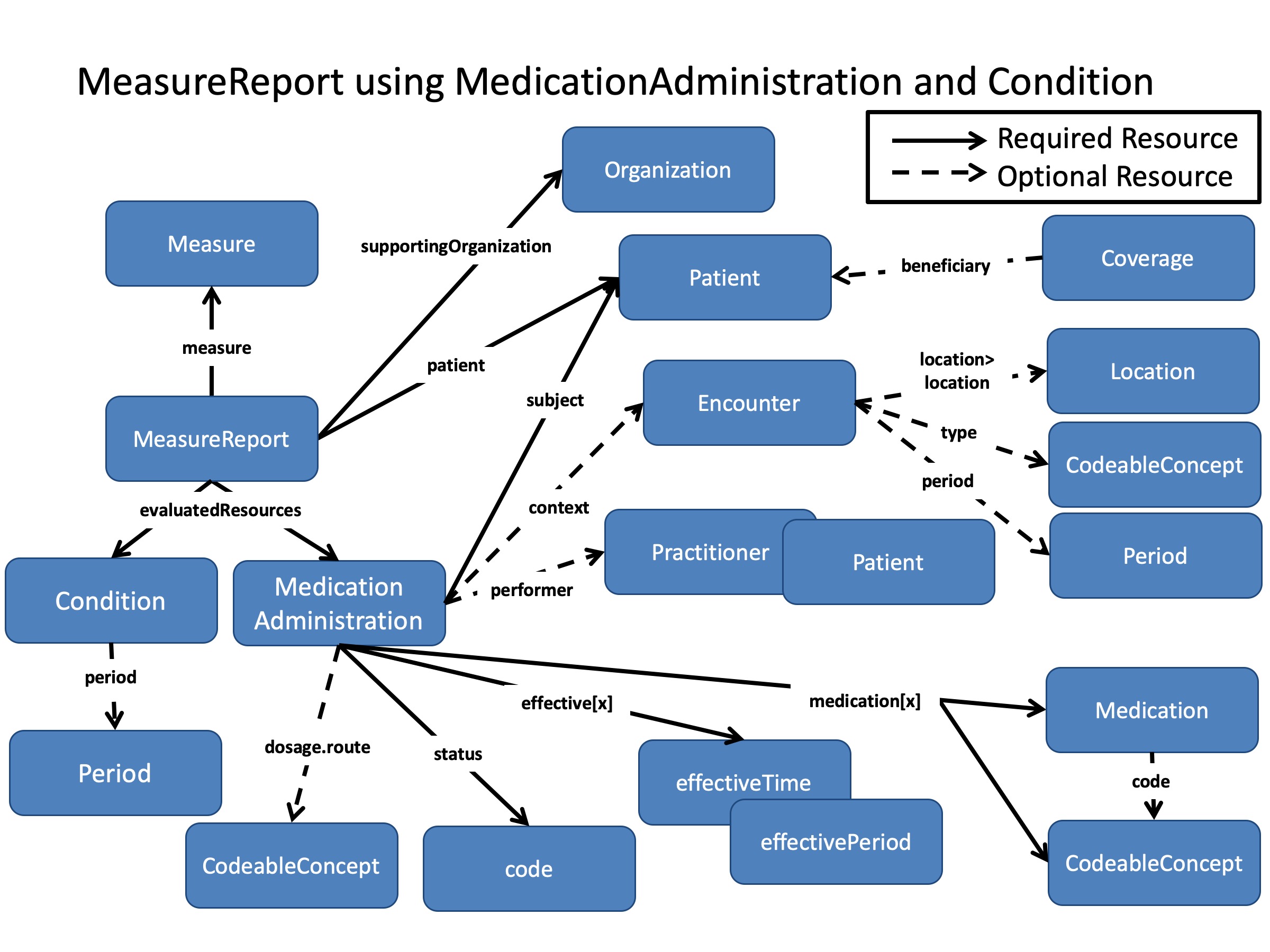
Option 1: Measure Report Using MedicationAdministration
VTE-1 has been met when a patient:
- has an inpatient encounter such as for a joint replacement procedure
- is not pregnant or currently diagnosed with a venous thromboembolism
- is administered either Heparin, a Factor Xa Inhibitor, or Warfarin on the calendar day of admission or the day after.
The medications that qualify for the measure are listed in the value sets of codes in the measure documentation. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport when the patient has been administered one of these medications to meet the measure.
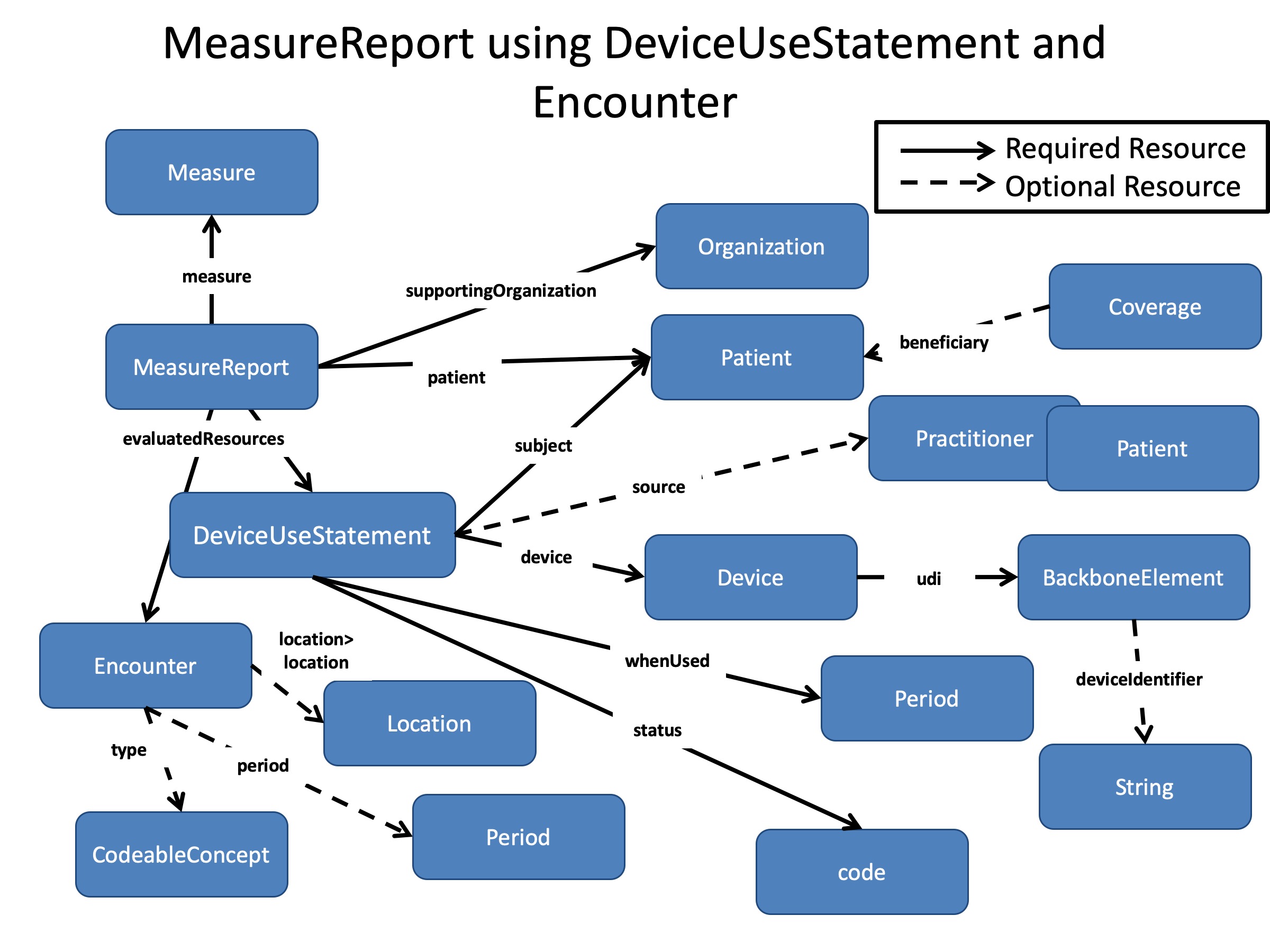
Option 2: Measure Report Using DeviceUseStatement and Encounter
VTE-1 has been met when a patient:
- has an inpatient encounter such as for a joint replacement procedure
- is not pregnant or currently diagnosed with a venous thromboembolism
- has a device to prevent venous thromboembolism prophylaxis on the calendar day of admission or the day after.
The devices that qualify for the measure are listed in the value sets of codes in the measure documentation. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport when the patient has had one of these Devices applied to meet the measure.
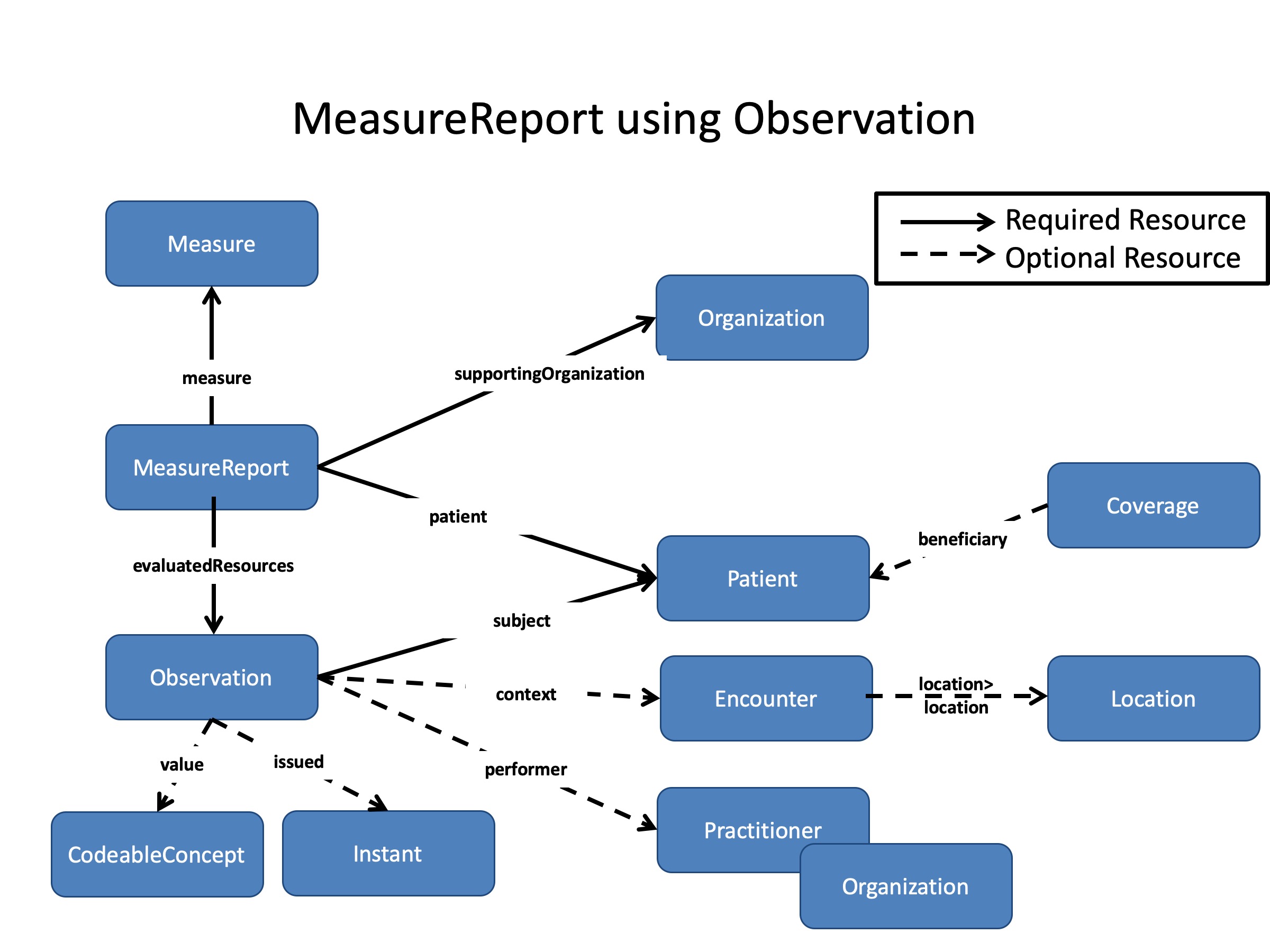
Option 3: Measure Report Using Observation
VTE-1 has been met when a patient:
- has an inpatient encounter such as for a joint replacement procedure
- is not pregnant or currently diagnosed with a venous thromboembolism
- and has been assessed to have a low risk for venous thromboembolism prophylaxis typically through laboratory testing, on the calendar day of admission or the day after.
The result codes that qualify as “low risk for VTE” are listed in the value sets of codes in the measure documentation. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport when the patient has had this Observation made to meet the measure.
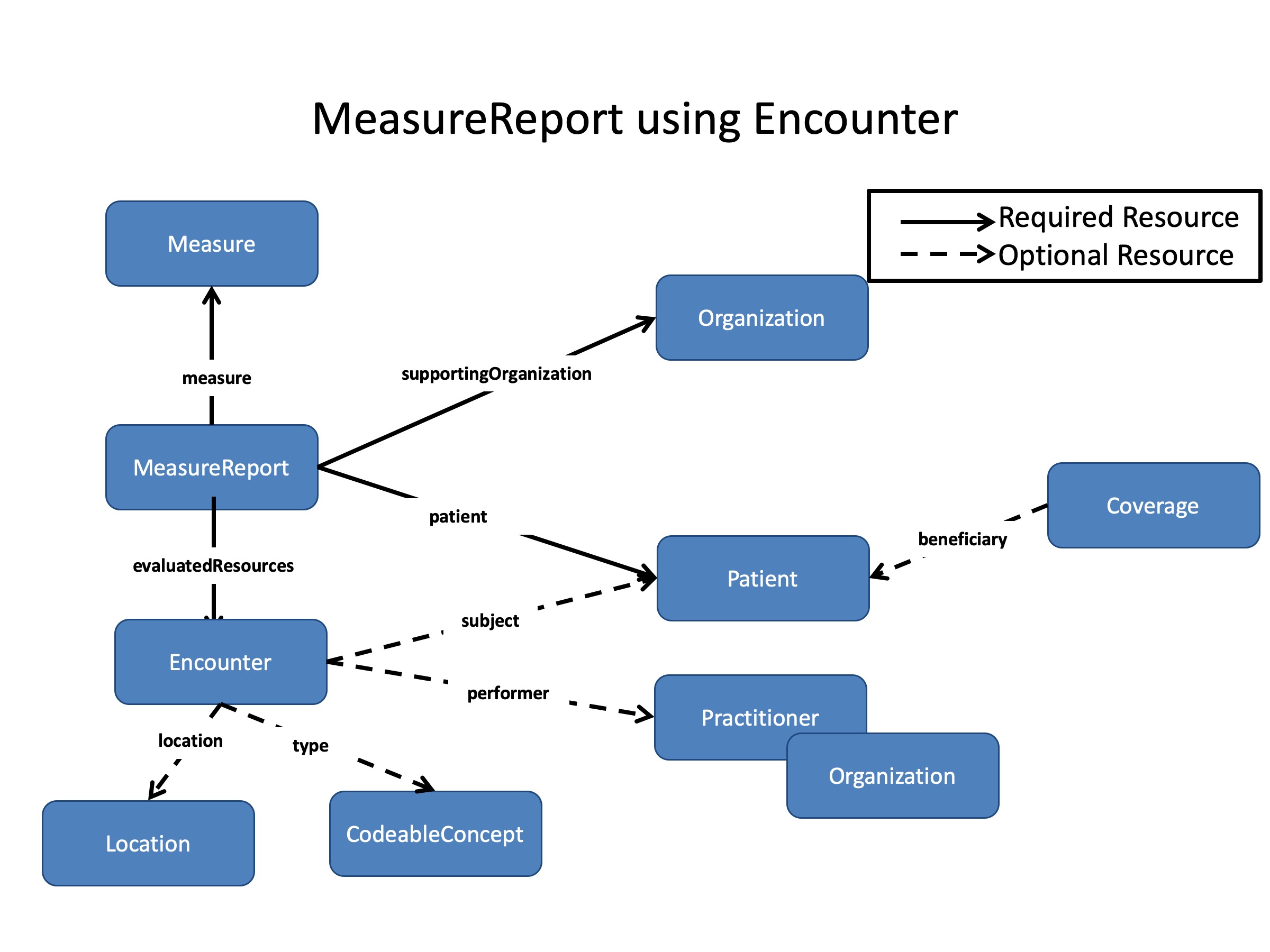
Option 4: Measure Report Using Encounter
When a patient has an inpatient encounter where the encounter is <2 days long, or when the encounter includes an ICU stay of 1 or more days, the patient can be can be excluded from the denominator of the measure. Codes for the ICU facility location will come from the HL7 ServiceDeliveryLocationRoleType valueset. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport when the patient when the patient has these types of encounters.
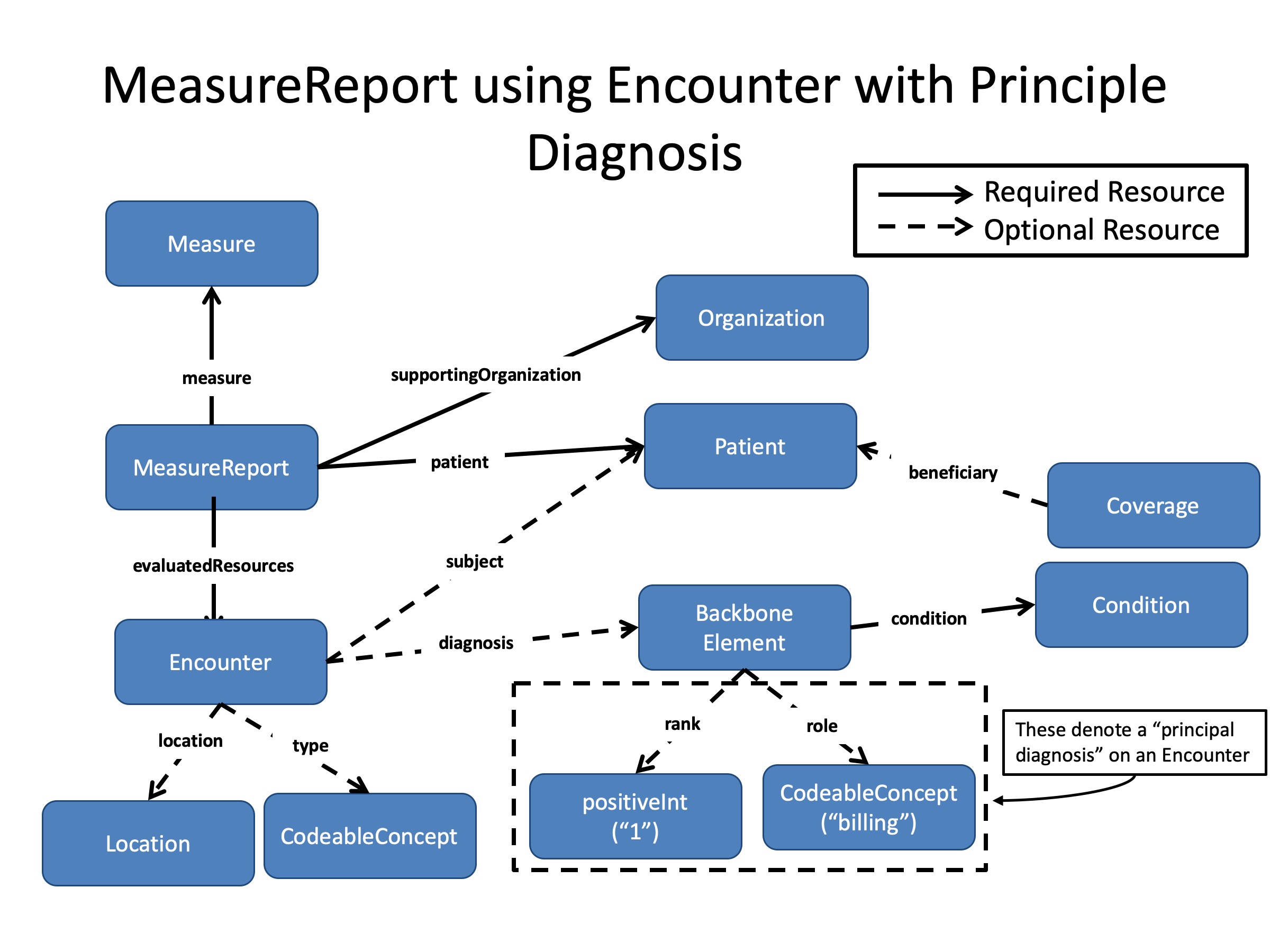
Option 5: Measure Report Using Encounter and Principle Diagnosis
When a patient has an inpatient encounter and is principally diagnosed with either a mental health condition, or a stroke (either hemorrhagic or ischemic), they are excluded from the denominator of the measure. Codes for the diagnoses will come from the respective valuesets from the measure. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport when the patient has had this Encounter with these principle diagnosis.
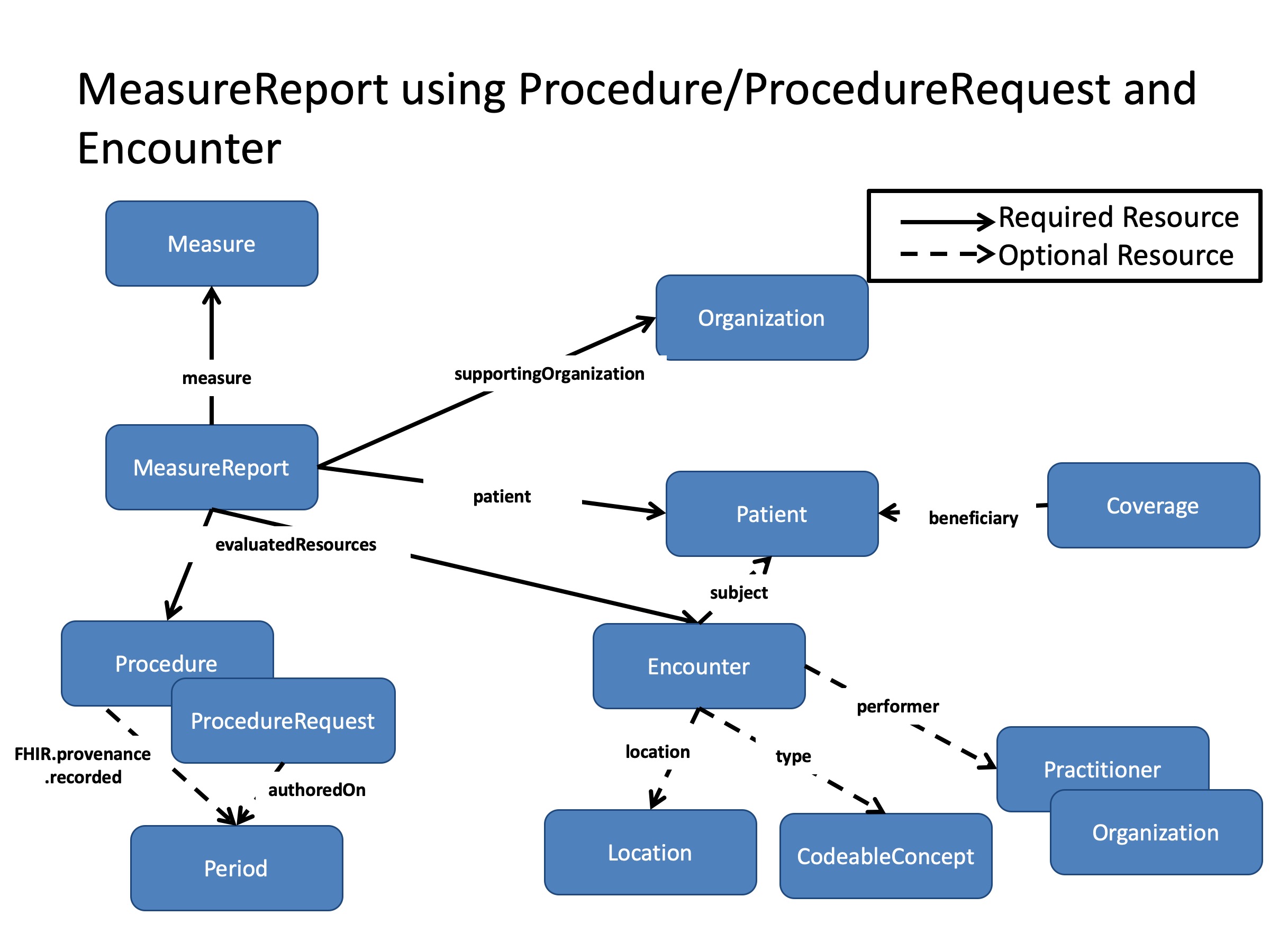
Option 6: Measure Report Using Procedure/ProcedureRequest and Encounter
When a patient has an inpatient encounter, during which they are provided Comfort Measures within 1 day of being admitted or 1 day of a surgical procedure for which they were admitted, these Comfort Measures are excluded from the denominator of the measure. for the measure. The surgical procedure is defined by the presence of a code from the “general or neuraxial anesthesia” value set present in the measure. The Comfort measures are represented by either a Procedure or a ProcedureRequest with a code from the “Comfort Measures” value set present in the measure. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport when the patient has had intervention comfort measures.
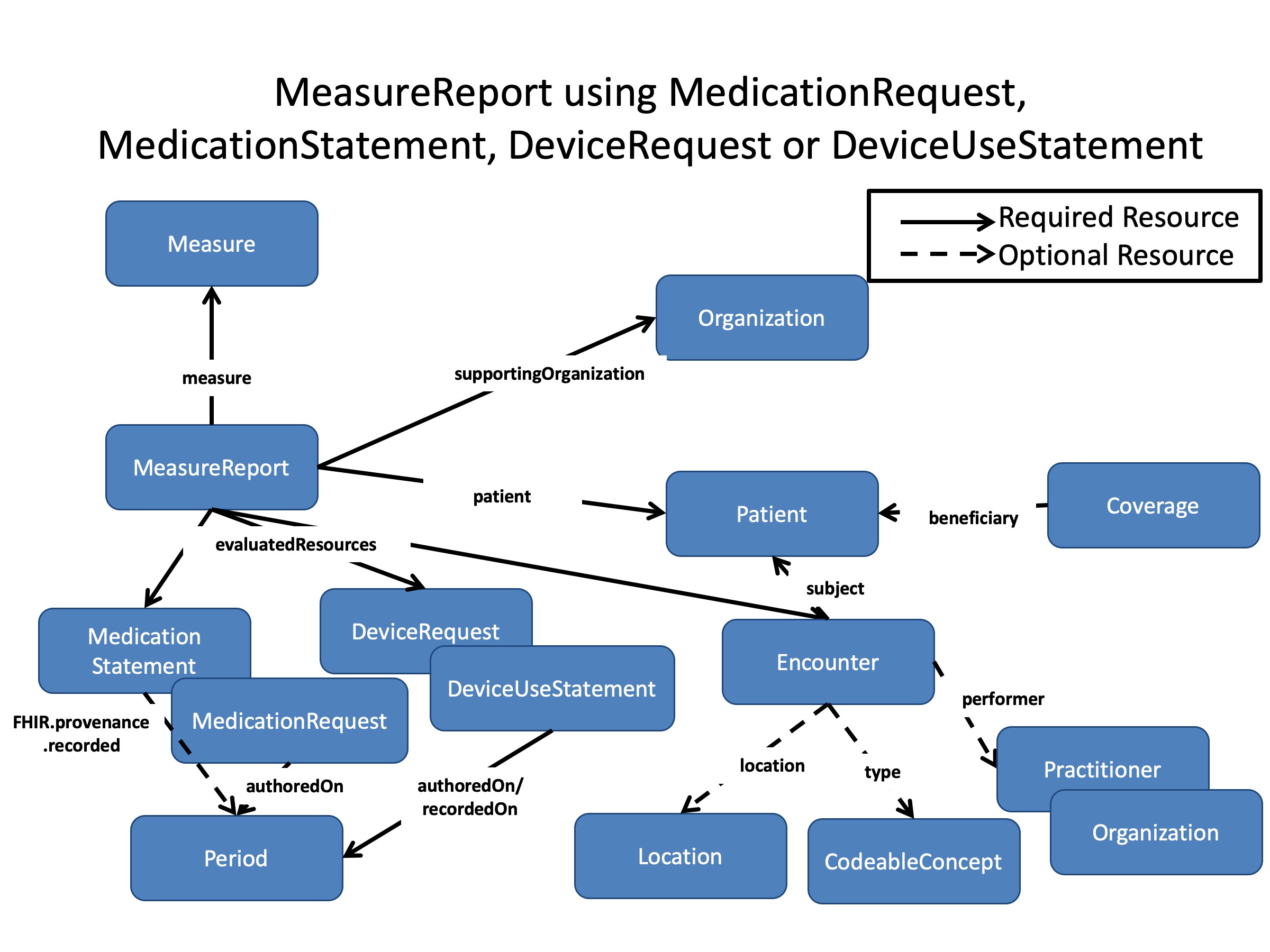
Option 7: Measure Report Using MedicationRequest, DeviceRequest, MedicationStatement or DeviceUseStatement
When a patient has an inpatient encounter, during which they should be given venous thromboembolism prophylaxis, but they are not given said prophylaxis, the patient’s record must document a reason the medication/device was not provided. This reason must be coded, and must come from either the “medical reason” or “patient refusal” value sets, as stated in the measure logic. If these criteria are met, the patient will have been found to satisfy the requirements of the measure. The following resource graph diagram shows what would be included with a DEQM Individual MeasureReport to meet the measure when the venous thromboembolism prophylaxis was not done, for example because of patient refusal.
VTE-1 Measure Reporting Interactions
Individual MeasureReport
Reporter pushes the Bundle of supporting resource with VTE-1 Individual MeasureReport Bundle to the end user.
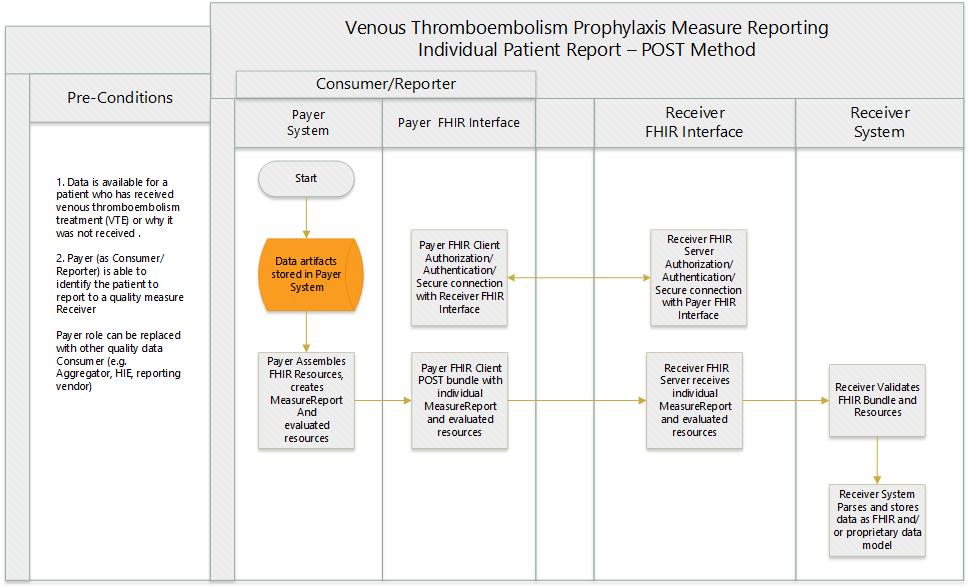
Examples
Scenario:
Payer X who is acting in the role of a Reporter submits a VTE Individual Report for Patient P to Receiver Z. The body of the request is a transaction bundle including the Individual MeasureReport and all the related resources containing the relevant data used to compute the CQM criteria. An HTTP Status success code is returned on successful submission.
POST Summary Report
POST [base]
Request body
{
"resourceType": "Bundle",
"type": "transaction",
"entry": [
{
"fullUrl": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc4",
"resource": {
"resourceType": "MeasureReport",
"status": "complete",
"type": "individual",
"measure": {
"reference": "Measure/measure-vte"
},
"patient": {
"reference": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc6"
},
"date": "2019-03-14",
"reportingOrganization": {
"reference": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc5"
},
"period": {
"end": "2018-01-01",
"start": "2018-12-31"
},
"group": [
{
"population": [
{
"code": {
"coding": [
{
"system": "http://hl7.org/fhir/measure-population",
"code": "initial-population",
"display": "Initial Population"
}
]
}
},
{
"code": {
"coding": [
{
"system": "http://hl7.org/fhir/measure-population",
"code": "numerator",
"display": "Numerator"
}
]
}
},
{
"code": {
"coding": [
{
"system": "http://hl7.org/fhir/measure-population",
"code": "denominator",
"display": "Denominator"
}
]
}
}
],
"measureScore": 100
}
]
},
"request": {
"method": "POST",
"url": "MeasureReport"
}
},
{
"fullUrl": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc5",
"resource": {
"resourceType": "Organization",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/organization-deqm"
]
},
"identifier": [
{
"use": "official",
"type": {
"coding": [
{
"system": "http://hl7.org/fhir/v2/0203",
"code": "TAX",
"display": "Tax ID number"
}
]
},
"system": "urn:oid:2.16.840.1.113883.4.2",
"value": "123456789",
"assigner": {
"display": "www.irs.gov"
}
}
],
"active": true,
"type": [
{
"coding": [
{
"system": "http://hl7.org/fhir/organization-type",
"code": "prov",
"display": "Healthcare Provider"
}
]
}
],
"name": "DaVinciHospital01",
"telecom": [
{
"system": "phone",
"value": "(+1) 401-555-1212"
}
],
"address": [
{
"line": [
"73 Lakewood Street"
],
"city": "Warwick",
"state": "RI",
"postalCode": "02886",
"country": "USA"
}
]
},
"request": {
"method": "POST",
"url": "Organization"
}
},
{
"fullUrl": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc6",
"resource": {
"resourceType": "Patient",
"meta": {
"profile": [
"http://hl7.org/fhir/us/qicore/StructureDefinition/qicore-patient"
]
},
"extension": [
{
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-birthsex",
"valueCode": "F"
},
{
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-race",
"extension": [
{
"url": "ombCategory",
"valueCoding": {
"system": "urn:oid:2.16.840.1.113883.6.238",
"code": "2106-3",
"display": "White"
}
},
{
"url": "text",
"valueString": "White"
}
]
},
{
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-ethnicity",
"extension": [
{
"url": "ombCategory",
"valueCoding": {
"system": "urn:oid:2.16.840.1.113883.6.238",
"code": "2186-5",
"display": "Not Hispanic or Latino"
}
},
{
"url": "text",
"valueString": "Not Hispanic or Latino"
}
]
}
],
"identifier": [
{
"use": "usual",
"type": {
"coding": [
{
"system": "http://hl7.org/fhir/v2/0203",
"code": "MR",
"display": "Medical record number"
}
]
},
"system": "http://hospital.davinci.org",
"value": "67890"
}
],
"active": true,
"name": [
{
"use": "official",
"family": "Webster",
"given": [
"Thelma"
]
}
],
"gender": "female",
"birthDate": "1948-04-28",
"deceasedBoolean": false,
"address": [
{
"use": "home",
"line": [
"7496 Beaver Ridge Ave"
],
"city": "Thornton",
"state": "NJ",
"postalCode": "07003",
"country": "USA"
}
],
"maritalStatus": {
"coding": [
{
"system": "http://hl7.org/fhir/v3/MaritalStatus",
"code": "M",
"display": "Married"
}
]
},
"communication": [
{
"language": {
"coding": [
{
"system": "urn:ietf:bcp:47",
"code": "en-US",
"display": "US English"
}
]
},
"preferred": true
}
]
},
"request": {
"method": "POST",
"url": "Patient"
}
},
{
"fullUrl": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc7",
"resource": {
"resourceType": "Encounter",
"meta": {
"profile": [
"http://hl7.org/fhir/us/qicore/StructureDefinition/qicore-encounter"
]
},
"status": "finished",
"class": {
"system": "http://hl7.org/fhir/encounter-class",
"code": "inpatient",
"display": "inpatient"
},
"type": [
{
"coding": [
{
"system": "http://snomed.info/sct",
"code": "32485007",
"display": "Hospital admission"
}
]
}
],
"subject": {
"reference": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc6"
},
"period": {
"start": "2018-07-19T11:00",
"end": "2018-07-19T:14:30"
},
"location": [
{
"location": {
"reference": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc8",
"display": "Mother Charity Hospital"
}
}
],
},
"request": {
"method": "POST",
"url": "Encounter"
}
},
{
"fullUrl": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc8",
"resource": {
"resourceType": "Location",
"identifier": [
{
"use": "official",
"system": "http://www.hl7.org/oid/",
"value": "1.2.3.4.181"
}
],
"status": "active",
"name": "Mother Charity Hospital",
"mode": "instance",
"telecom": [
{
"system": "phone",
"value": "(313) 555-5671",
"use": "work"
}
],
"address": {
"use": "work",
"type": "physical",
"line": [
"869 W Oak Street"
],
"city": "Royal Oak",
"district": "Oakland County",
"state": "MI",
"postalCode": "48073"
},
"physicalType": {
"coding": [
{
"system": "http://hl7.org/fhir/location-physical-type",
"code": "bu",
"display": "Building"
}
]
}
},
"request": {
"method": "POST",
"url": "Location"
}
},
{
"fullUrl": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc9",
"resource": {
"resourceType": "MedicationAdministration",
"status": "completed",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "1658634",
"display": "0.5 ML heparin sodium, porcine 10000 UNT/ML Injection"
}
]
},
"subject": {
"reference": "urn:uuid:b5cf5a8c-63f0-437f-84fd-dc8a3cf43cc6"
},
"effectivePeriod": {
"start": "2018-07-19T12:00",
"end": "2018-07-19T12:00"
},
"dosage": {
"route": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "34206005",
"display": "Subcutaneous route"
}
]
}
}
}
}
]
}
Response
HTTP/1.1 200 OK
[other headers]



