This page is part of the US Core (v7.0.0-ballot: STU7 Ballot) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 8.0.1. For a full list of available versions, see the Directory of published versions. Page versions: R8 R7
| Page standards status: Informative |
This page documents requirements common to all US Core actors used in this guide. The conformance verbs - SHALL, SHOULD, MAY - used in this guide are defined in FHIR Conformance Rules.
The Profiles and Extensions page list the US Core Profiles and have been defined for this implementation guide. US Core Profile StructureDefinitions defines the minimum elements, extensions, vocabularies, and ValueSets that SHALL be present and constrains the way the elements are used when using the profile. Each US Core Profile page has a “Quick Start” guide to the supported FHIR RESTfUL transactions for each profile
The US Core Profile elements include Mandatory, Must Support, and Additional USCDI Requirements. Mandatory elements are required and have a minimum cardinality of 1 (min=1). Must Support element server and client expectations are defined by US Core. Additional USCDI Requirements elements are neither Mandatory nor Must Support but designated USCDI Requirements for ONC Health IT Certification and, for certified systems, are equivalent to Must Support elements. All Mandatory, Must Support, or Additional USCDI Requirements are in-scope for ONC Health IT Certification (g(10) certification) testing. The Must Support page defines the server and client expectations for processing these different element requirements and illustrates how they are displayed and documented.
The Capability Statements page outlines conformance requirements and expectations for the US Core Servers and Client applications. In addition, the US Core Server CapabilityStatement and US Core Client CapabilityStatement identify the specific profiles and RESTful transactions that need support. The US Core Profiles identify the structural constraints, terminology bindings, and invariants. Similarly, each US Core SearchParameter and Operation resources specify how the server understands them. However, implementers must refer to the CapabilityStatement for details on the RESTful transactions, specific profiles, and the search parameters applicable to each US Core actor.
There are two different ways to implement US Core:
Systems may deploy and support one or more US Core Profiles to represent clinical information. They use the profile’s content model without any expectations to implement the US Core interactions.
An example scenario would be a server using only the FHIR Bulk Data Access (Flat FHIR) approach to export the US Core Data for Interoperability resources. For this server, the US Core interactions are unnecessary.
To support a US Core Profile, a server:
CapabilityStatement.rest.resource.supportedProfile element
the US Core Profile’s official or “canonical” URL is located on each US Core Profile page
example CapabilityStatement snippet for a server supporting the US Core Patient Profile:
{
"resourceType": "CapabilityStatement",
...
"rest": [
{
"mode": "server",
...
"resource": [
...
{
"type": "Patient",
"supportedProfile": [
"http://hl7.org/fhir/us/core/StructureDefinition/us-core-patient"
],
...
}
]
}
]
}
Servers may deploy and support one or more US Core Profiles to represent clinical information and one or more of the following US Core interactions:
Servers implementing both can claim conformance to the US Core Profile content structure and the RESTful interactions defined by implementing all or parts of the US Core CapabilityStatement into their capabilities as described below. A server that certifies to the 21st Century Cures Act for accessing patient data must implement all components in the USCDI and the US Core CapabilityStatement.
A conformant server:
SHOULD declare conformance with the US Core Server Capability Statement by including its official URL in the server’s CapabilityStatement.instantiates element: http://hl7.org/fhir/us/core/CapabilityStatement/us-core-server
CapabilityStatement.rest.resource.supportedProfile element
Example CapabilityStatement snippet for a server conforming to the US Core Patient Profile:
{
"resourceType": "CapabilityStatement",
...
"instantiates": [
"http://hl7.org/fhir/us/core/CapabilityStatement/us-core-server"
],
...
"rest": [
{
"mode": "server",
...
"resource": [
...
{
[
{
"extension": [
{
"url": "required",
"valueString": "birthdate"
},
{
"url": "required",
"valueString": "name"
}
],
"url": "http://hl7.org/fhir/StructureDefinition/capabilitystatement-search-parameter-combination"
},
{
"extension": [
{
"url": "required",
"valueString": "family"
},
{
"url": "required",
"valueString": "gender"
}
],
"url": "http://hl7.org/fhir/StructureDefinition/capabilitystatement-search-parameter-combination"
},
{
{
"url": "required",
"valueString": "birthdate"
},
{
"url": "required",
"valueString": "family"
}
],
"url": "http://hl7.org/fhir/StructureDefinition/capabilitystatement-search-parameter-combination"
},
{
"extension": [
{
"url": "required",
"valueString": "gender"
},
{
"url": "required",
"valueString": "name"
}
],
"url": "http://hl7.org/fhir/StructureDefinition/capabilitystatement-search-parameter-combination"
}
]
}
]
"type": "Patient",
"supportedProfile": [
"http://hl7.org/fhir/us/core/StructureDefinition/us-core-patient"
],
"interaction": [
{
"code": "create"
},
{
"code": "search-type"
},
{
"code": "read"
}
],
"referencePolicy": [
"resolves"
],
"searchRevInclude": [
"Provenance:target"
],
"searchParam": [
{
"name": "_id",
"definition": "http://hl7.org/fhir/us/core/SearchParameter/us-core-patient-id",
"type": "token"
},
{
"name": "identifier",
"definition": "http://hl7.org/fhir/us/core/SearchParameter/us-core-patient-identifier",
"type": "token",
"documentation": "The client **SHALL** provide at least a code value and **MAY** provide both the system and code values.\n\nThe server **SHALL** support both."
},
{
"name": "name",
"definition": "http://hl7.org/fhir/us/core/SearchParameter/us-core-patient-name",
"type": "string"
}
],
...
}
]
}
]
}
The following rules summarize the requirements defined by FHIR Terminology for coded elements (CodeableConcept, Coding, and code datatypes).
Required binding to a ValueSet definition means that one of the codes from the specified ValueSet SHALL be used. For CodeableConcept, which permits multiple codings and a text element, this rule applies to at least one of the codings, and only text is not valid.
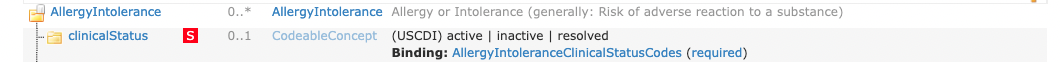
For example, the US Core AllergyIntolerance Profile clinicalStatus element has a required binding to the AllergyIntoleranceClinicalStatusCodes ValueSet. Therefore, when claiming conformance to this profile:
AllergyIntolerance.clinicalStatus.code.US Core Requestors SHALL be capable of processing the code in AllergyIntolerance.clinicalStatus.code.
Because of the FHIR conformance rule:
If an extensible binding is applied to an element with maximum cardinality > 1, the binding applies to all the elements. (Terminology Binding Extensible)
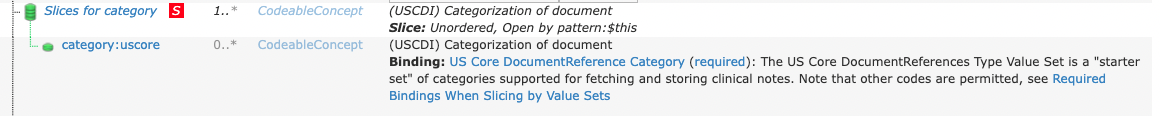
FHIR profiles use slicing when a coded element is a repeating element, and a particular ValueSet is desired for at least one of the repeats. This is a special case where a required ValueSet binding is used to differentiate the repeat. In this guide, the minimum cardinality for these ‘slices’ is set to 0 so that other codes are allowed when no suitable code exists in the ValueSet (equivalent to Extensible Binding below). Note that slicing by valueset does not affect the over the wire structure or validation of instances of these resources. The example in Figure 2 below illustrates this structure for the repeating DocumentReference.category element:
This structure, by being 0..*, allows servers to send concepts, not in the required ValueSet.
Extensible Binding means that one of the codes from the specified ValueSet SHALL be used if an applicable concept is present. If no suitable code exists in the ValueSet, alternate code(s) may be provided. For CodeableConcept, which permits multiple codings and a text element, this rule applies to at least one of the codings, and if only text is available, then just text may be used.
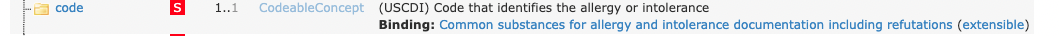
The US Core AllergyIntolerance Profile illustrates the extensible binding rules for CodeableConcept datatype. The AllergyIntolerance.code element has an extensible binding to the VSAC ValueSet “Common substances for allergy and intolerance documentation including refutations” Allergy. When claiming conformance to this profile:
AllergyIntolerance.code.code if the concept exists in the ValueSetUS Core Requestors SHALL be capable of processing the code in AllergyIntolerance.code.code or text in AllergyIntolerance.code.text
Although the FHIR guidance for extensible bindings indicates that all conceptual overlaps including free text, be mapped to the coded values in the bindings, US Core guidance provides more flexibility for situations where implementers cannot fully comply with the FHIR guidance. This flexibility is sometimes necessary and expected for legacy and text-only data. However, for newly recorded, non-legacy data, a system SHOULD adhere to the extensible binding rules.
For example, the US Core Procedure Codes and US Core Condition Codes ValueSets contain several high-level abstract codes. For data not captured by the system transmitting the information, the coded data SHOULD be automatically converted to fine-grained codes from the specified ValueSet. If this is not possible, the system can provide the existing code or the free text, and a high-level abstract code, such as SNOMED CT ‘Procedure’, to remain conformant with the extensible binding.
Alternate codes may be provided in addition to the standard codes defined in required or extensible ValueSets. The alternate codes are called “translations”. These translations may be equivalent to or narrower in meaning than the standard concept code.
Example of multiple translations for Body Weight concept code.
"code": {
"coding": [
{
"system": "http://loinc.org", //NOTE:this is the standard concept defined in the ValueSet//
"code": "29463-7",
"display": "Body Weight"
},
//NOTE:this is a translation to a more specific concept
{
"system": "http://loinc.org",
"code": "3141-9",
"display": "Body Weight Measured"
},
//NOTE:this is a translation to a different code system (Snomed CT)
{
"system": "http://snomed.info/sct",
"code": "364589006",
"display": "Body Weight"
}
//NOTE:this is a translation to a locally defined code
{
"system": "http://AcmeHealthCare.org",
"code": "BWT",
"display": "Body Weight"
}
],
"text": "weight"
},
Example of translation of CVX vaccine code to NDC code.
"vaccineCode": {
"coding": [
{
"system" : "http://hl7.org/fhir/R4/sid/cvx",
"code": "158",
"display": "influenza, injectable, quadrivalent"
},
{
"system" : "http://hl7.org/fhir/R4/sid/ndc",
"code": "49281-0623-78",
"display" : "FLUZONE QUADRIVALENT"
}
]
},
A FHIR modifier element is an element that modifies the meaning of a resource element. Although servers and clients SHALL be able to process Mandatory or Must Support elements, not all modifier elements are Mandatory or Must Support, and there is no requirement for supporting them. Therefore, FHIR clients need to be aware of unexpected modifier elements in the data they receive because they can alter the meaning of the data and can potentially lead to errors or even security risks if not properly handled. In addition, modifiers can be introduced when the data is created, edited, or transmitted, so it is crucial to ensure that all modifiers are understood and handled correctly.
In addition to declaring which US Core profiles they support, Servers MAY communicate a system-wide profile in their CapabilityStatement to identify which additional elements, including modifier elements, they support. However, systems are free to include other data elements - and receivers SHOULD accept instances that even contain unexpected data elements except when those elements are modifier elements. Unless a client determines they can process it safely, rejection is typically the only safe action if unexpected modifier elements are present. For example, an app or system may process modifier elements nested inside an ignored element or in a resource only for human review.
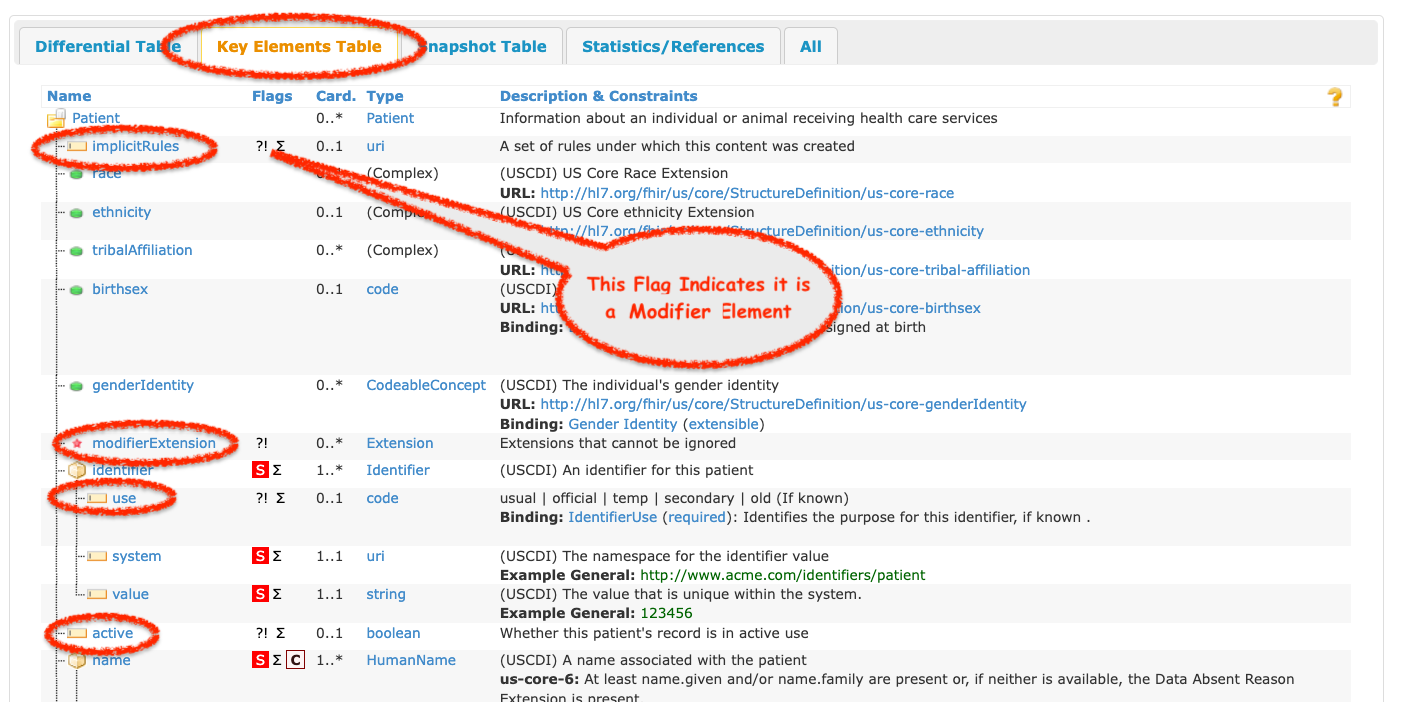
Some examples of modifiers that are not Must Support elements in US Core Profiles include:
implicitRules element common to all profilesmodifierExtension element common to all profilesObservation.value[x].comparatorPractitioner.identifier.usePatient.activeImplementers SHOULD review the “Key Elements Tab” on the US Core profile pages. This view lists all the Must Support and the modifier elements for a profile, as demonstrated in Figure 4 below.
There are situations when information on a particular data element is missing, and the source system does not know the reason for the absence of data. If the source system does not have data for an element with a minimum cardinality = 0 (including elements labeled Must Support), the data element SHALL be omitted from the resource. However, if the data element is a Mandatory element (in other words, where the minimum cardinality is > 0), it SHALL be present even if the source system does not have data. The core specification guides what to do in this situation, which is summarized below:
unknown - The value is expected to exist but is not known.Example: Patient resource where the patient name is not available.
{
"resourceType": "Patient",
...
"name": [
{
"extension": [
{
"url": "http://hl7.org/fhir/StructureDefinition/data-absent-reason",
"valueCode": "unknown"
}
]
}
]
"telecom":
...
}
text element is used.
display element.unknown from the DataAbsentReason Code System.Example: CareTeam resource where the mandatory CareTeam.participant.role value is unknown.
...
"participant": [
{
"role": [
{
"coding": [
{
"url": "http://hl7.org/fhir/StructureDefinition/data-absent-reason",
"code": "unknown",
"display": "unknown"
}
]
}
],
"member": {
"reference": "Practitioner/practitioner-1",
"display": "Ronald Bone, MD"
}
},
...
if the ValueSet does not have the appropriate “unknown” concept code, you must use a concept from the ValueSet otherwise, the instance will not be conformant
AllergyIntolerance.clinicalStatus*Condition.clinicalStatus*DocumentReference.statusImmunization.statusGoal.lifecycleStatus*The clinicalStatus element is conditionally mandatory based on resource-specific constraints.
If any of these status code is missing, a 404 HTTP error code and an OperationOutcome SHALL be returned in response to a read transaction on the resource. If returning a response to a search, the problematic resource SHALL be excluded from the search set, and a warning OperationOutcome SHOULD be included indicating that other search results were found but could not be compliantly expressed and have been suppressed.
The FHIR RESTful Search API requires that servers that support search SHALL support the HTTP POST based search. For all the supported search interactions in this guide, servers SHALL also support the GET based search.
token type searchparameter (how to search by token)
reference type searchparameter (how to search by reference)
date type searchparameter (how to search by date):
date and to the second + time offset for elements of datatype dateTime.date and to the second + time offset for elements of datatype dateTime.The table below summarizes the date precision:
| SearchParameter | Element Datatype | Minimum Date Precision | Example |
|---|---|---|---|
| date | date | day | GET [base]/Patient?family=Shaw&birthdate=2007-03-20 |
| date | dateTime, Period | second + time offset | GET [base]Observation?patient=555580&category=laboratory&date=ge2018-03-14T00:00:00-08:00 |
Servers are strongly encouraged to support a query for resources without requiring a status parameter. However, if business requirements prohibit this, they SHALL follow the guidelines here.
For searches where the client does not supply a status parameter, an implementation’s business rules may override the FHIR RESTful search expectations and require a status parameter to be provided. These systems are allowed to reject such requests as follows:
400 statusIf a system doesn’t support a specific status code value that is queried, it SHOULD return an HTTP 200 status with a search bundle. The search bundle SHOULD contain resources matching the search criteria and an OperationOutcome warning the client which status code value is not supported.
For example, in a query enumerating all the AllergyIntolerance.verificationStatus statuses to a system that supports concepts unconfirmed, confirmed, and entered-in-error but not the concept refuted, the search parameter is referring to an unsupported code since refuted is not known to the server.
Storyboard for this example
This example is based upon the following scenario:
Patient 1137192 uses an App to request all his encounters from the provider. The provider system requires status and rejects the request returning a 400 and an OperationOutcome specifying that a status parameter is required for this search.
Request:
Get “all encounters” for a patient 1137192 by querying Encounter using the patient search parameter.
GET [base]/Encounter?patient=1137192
Response:
Instead of returning a search Bundle resource containing all the Encounter for the patient, the server return a 400 Not Found and an OperationOutcome detailing that a status parameter is required for this search.
HTTP/1.1 400 Not Found
[other headers]
{
"resourceType": "OperationOutcome",
"id": "no-status",
"issue": [
{
"severity": "error",
"code": "business-rule",
"details": {
"text": "A \"status\" search parameter is required for this search"
},
"diagnostics": "valid statuses for Encounter include planned | arrived | triaged | in-progress | onleave | finished | cancelled | entered-in-error | unknown"
}
]
}
CapabilityStatement.rest.resource.interaction.documentation.