This page is part of the PACIO Advance Directive Information Implementation Guide (v2.0.0-ballot: STU 2 Ballot) based on FHIR (HL7® FHIR® Standard) R4. This version is a pre-release. The current official version is 1.0.0. For a full list of available versions, see the Directory of published versions
| Page standards status: Informative |
Content Type 3, are Portable Medical Orders (such as a DNR and/or POLST/MOLST orders). These documents tell other healthcare professionals what the treatment intervention preferences are for a person, and are usually intended to be created when there is an expectation of a limited life-expectancy. Portable medical order documents are authored by practitioners, not patients, and are legal physician orders. They do not document goals, preferences, and priorities that a patient intends to be referenced as guidance when making care decisions but instead focus on medical treatment intervention decisions that already have been made so as to guide treatment interventions.
All doctors, emergency medical professionals, and other healthcare professionals, must follow these portable medical orders as the person moves from one location to another (hospital, care facility, home, etc.), unless another practitioner examines the person, reviews the orders with the person or their healthcare agent, and a decision is reached that changes to the orders are warranted or desired. In an emergency situation, life-sustaining procedures that are normally required of emergency response personnel will be overridden by the contents of portable medical orders.
Depending on the state, portable medical orders may be known by any of the following names:
Portable medical orders are not advance directives and should not be confused with them:
These are important distinctions to understand.
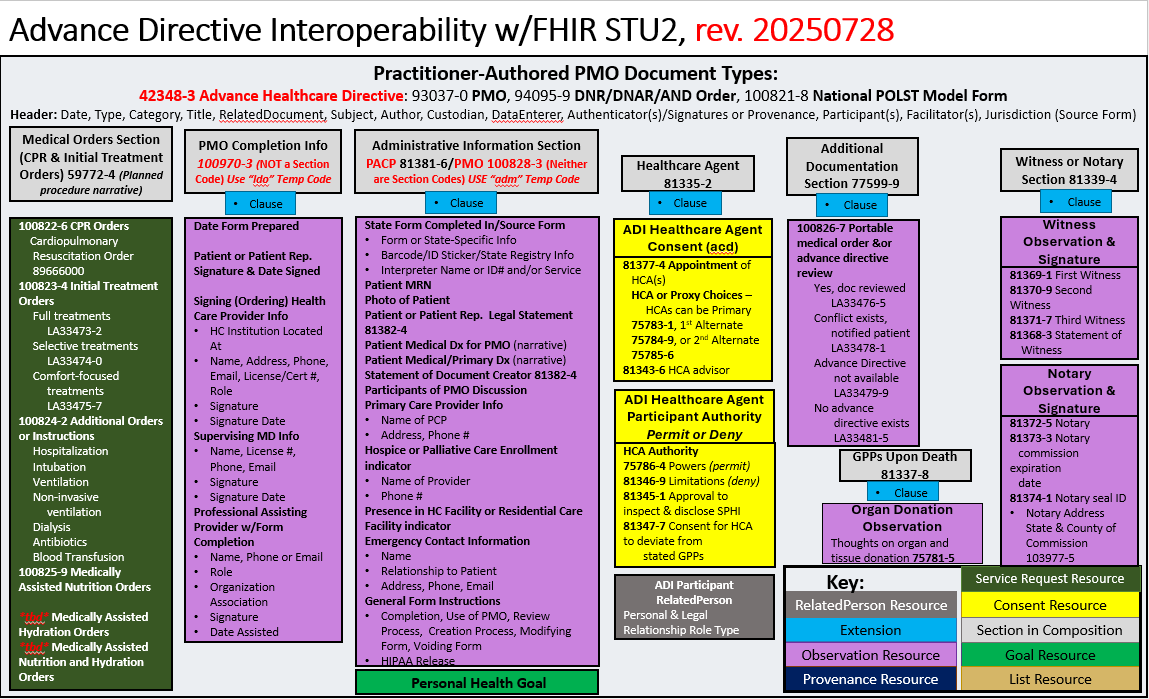
Structurally, the document structure shares the same ADI header as the PACP document and includes sections specific to the portable medical order (PMO):
The following story continues the Content Type 1 user story for person-authored advance healthcare directives such as advance care plans or jurisdictional advance directives, which may be found in a single consolidated document or segmented into two documents, one for designation of a durable medical power of attorney and the other for expressing treatment preferences called a living will.
Betsy Smith-Johnson is a 74-year old female, who lives in Michigan with her son Charles and his wife Lisa, who are her designated primary and backup healthcare agents. She understands that documenting her care experience and treatment intervention preferences, and designated healthcare agents, can inform care and treatment she would receive during a health crisis or emergency if she were unable to communicate with her care team.
She creates and stores a digital personal advance care plan (PACP) using a consumer-facing application, and due to her history of behavioral health conditions, she also completes a mental health advance directive (MHAD), on paper, that she is able to upload into the consumer-facing application. She ensures that both Charles and Lisa have access to her PACP and MHAD through a secure, patient-directed share link she initiates within the consumer-facing application. The consumer-facing application is connected to a secure, national advance care plan (ACP) document registry and repository that is accessible to health information exchanges, other providers, and personal health record applications, which gives Betsy confidence that her ACP documents will be available to treating providers and care settings that need to understand her values and goals of care as part of delivering care and creating a person-centered plan of care.
Betsy experiences a fall in the home and following an encounter in the emergency department, she is transferred to a skilled nursing facility (SNF) near her home to receive therapy and rehabilitation services so as to be able to return home. During that SNF stay, as part of her admission process, the SNF admission nurse and social worker work with Betsy to create a portable medical order (PMO) as appropriate for that jurisdiction and care setting. Betsy expresses a desire for CPR and full treatment, in case of an emergency or health crisis, and is focused on getting back home to Charles and Lisa and the life she values.
The SNF team uses a practitioner-facing application to create her PMO, which is reviewed with Betsy and signed off on by her SNF practitioner upon the initial visit. Once executed the document is stored in digital form in a secure, national ACP document registry and repository is connected to a national advance care plan (ACP) document registry and repository that is accessible to health information exchanges, other providers, and personal health record applications.
Betsy is discharged to home from the SNF, with home health services to ensure her transition to home is supported with the services she requires to continue her recovery. Her PACP, MHAD and PMO are retrieved by the home health system to inform the care and treatment she receives so as to ensure a person-centered plan of care is able to be created that is consistent with her values and goals of care.
Charles finds his mom, Betsy, sitting on the floor one day and believes she may have had another fall. However, when he gets her up and seated in a chair he notices that she is weak, disoriented and has slurred speech. He fears she has had a stroke, calls 9-1-1 and accompanies Betsy to the emergency department where the hospital is able to access her PMO, MHAD and PACP from their electronic health record to inform the care and treatment she receives. The stroke Charles suspects is confirmed and after receiving treatment, Betsy is discharged to her previous SNF for rehabilitation and therapy. The admissions team there is familiar with Betsy and uses their electronic health record to retrieve her ACP documents to guide the care she will receive. Betsy communicates with Charles, using verbal and non-verbal communication, to tell him she wants more comfort-focused care this time. Charles relays to the SNF team that she wants softer treatments, more comfort-focused and they work with Charles and Betsy to void the previous PMO and create a new one that is more representative of her current preferences.
As before, the SNF team’s practitioner-facing application is used to create the new PMO, which when reviewed with Charles and Betsy is then signed off on by her SNF practitioner and stored in a secure, national ACP document registry and repository that is accessible to health information exchanges, other providers, and personal health record applications.
Betsy and Charles consider that her PACP and MHAD need to be updated to align with her new goals of care, and they work together using the consumer-facing application Betsy had used previously to void the previous MHAD and update her PACP. Charles and Betsy fill out a new paper MHAD and upload it into the consumer-facing application. In the application they both see the new PMO, and Betsy instructs Charles to ensure access to that updated document is granted to himself and his wife Lisa, Betsy’s healthcare agents. The access granted to them previously enables them to see the new MHAD and updated PACP as well.
All of Betsy’s current ACP documents are accessible to treating care teams Betsy may have in the future, so they can inform her future care, and are also accessible to Charles, Lisa and Betsy herself through the national ACP document registry and repository and its connections to state health information exchanges, other providers, and personal health record applications.