This page is part of the Da Vinci Prior Authorization Support (PAS) FHIR IG (v1.0.0: STU 1) based on FHIR R4. The current version which supercedes this version is 1.1.0. For a full list of available versions, see the Directory of published versions 
This section of the implementation guide defines the specific conformance requirements for systems wishing to conform to this Prior Authorization Support implementation guide. The bulk of it focuses on the Claim $submit operation, though it also provides guidance on privacy, security and other implementation requirements.
Before reading this formal specification, implementers should first familiarize themselves with two other key portions of the specification:
The Use Cases & Overview page provides context for what this formal specification is trying to accomplish and will give a sense of both the business context and general process flow enabled by the formal specification below.
The Technical Background page provides information about the underlying specifications and indicates what portions of them should be read and understood to have necessary foundation to understand the constraints and usage guidance described here.
This implementation guide uses specific terminology to flag statements that have relevance for the evaluation of conformance with the guide:
SHALL indicates requirements that must be met to be conformant with the specification.
SHOULD indicates behaviors that are strongly recommended (and which may result in interoperability issues or sub-optimal behavior if not adhered to), but which do not, for this version of the specification, affect the determination of specification conformance.
MAY describes optional behaviors that are free to consider but where the is no recommendation for or against adoption.
This implementation guide sets expectations for two types of systems:
This specification makes significant use of FHIR profiles and terminology artifacts to describe the content to be shared as part of prior authorization requests and responses.
The full set of profiles defined in this implementation guide can be found by following the links on the Artifacts page.
NOTE FHIR uses a pair of resources called Claim and ClaimResponse for multiple purposes - they are used for actual claim submission, but they are also used for managing prior authorizations and pre-determinations. These are distinguished by the Claim.use code. All references to Claim and ClaimResponse in this implementation guide are using it for the prior authorization purpose.
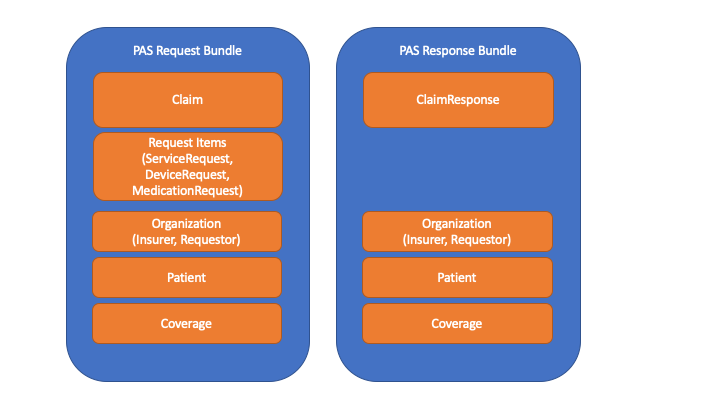
The primary interaction supported by this implementation guide is submitting a prior authorization request and receiving back a response. To perform this, a PASBundle resource is constructed by the client (EHR) system. That Bundle will contain a Claim resource (which FHIR uses to submit prior authorization requests), together with various referenced resources needed to support the population of the 5010 version of the ASC X12N 278 prior authorization request and the 6020 version of the ASC X12N 275 additional documentation transactions.
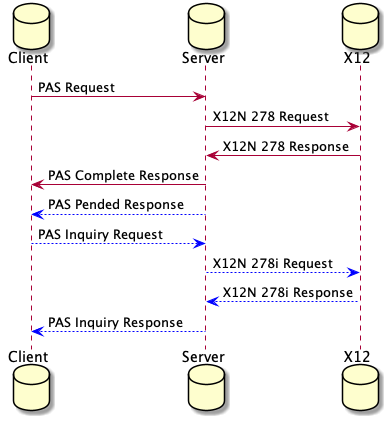
This Bundle will then be sent as the sole payload of a Claim/$submit operation. The system on which the operation is invoked will convert the Bundle into an ASC X12N 278 and 0..* additional unsolicited 275 transactions and execute them all against the target payer system. It will then take the resulting 278 response and convert it into a response FHIR Bundle containing a ClaimResponse and associated resources. All of this SHOULD happen synchronously with a maximum of 15 seconds between the user initiating the prior authorization request and seeing the resulting response - i.e. including network transmission time for request and response. (Less time is better.)
In the event that the prior authorization cannot be evaluated and a final response returned within the required timeframe, a response in which one or more of the requested authorization items are ‘pended’ will be returned. The client (or other interested systems - e.g. patient, caregiver or performing provider systems) can then query the endpoint for the final results using either a polling or subscription-based mechanism. During this period of time, the same $submit operation can be used to request cancellation or modification of the prior authorization.
The Claim/$submit operation is executed by POSTing a FHIR Bundle to the [base url]/Claim/$submit endpoint. The Bundle can be encoded in either JSON or XML. (Servers SHALL support both syntaxes.) The first entry in the Bundle SHALL be a Claim resource complying with the profile defined in this IG to ensure the content is sufficient to appropriately populate an X12N 278 message. Additional Bundle entries SHALL be populated with any resources referenced by the Claim resource (and any resources referenced by those resources, fully traversing all references and complying with all identified profiles). Note that even if a given resource instance is referenced multiple times, it SHALL only appear in the Bundle once. E.g., if the same Practitioner information is referenced in multiple places, only one Practitioner instance should be created - referenced from multiple places as appropriate. Bundle.entry.fullUrl values SHALL be:
All GUIDs used SHALL be unique, including across independent prior authorization submissions - with the exception that the same resource instance being referenced in distinct prior authorization request Bundles can have the same GUID.
In addition to these core elements needed to populate the 278 message, any “supporting information” resources needed to process the prior authorization request (whether determined by DTR processes or by other means) must also be included in the Bundle. Relevant resources referenced by those “supporting information” resources SHALL also be included (e.g. prescriber Practitioner and Medication for a MedicationRequest). Any such resource that has a US Core profile SHALL comply with the relevant US Core profiles. All “supporting information” resources included in the Bundle SHALL be pointed to by the Claim resource using the Claim.supportingInfo.valueReference element. To attach PDFs, CDAs, JPGs, a DocumentReference instance should be used. The Claim.supportingInfo.sequence for each entry SHALL be unique within the Claim.
All resources SHALL comply with their respective profiles. FHIR elements not marked as ‘must support’ MAY be included in resources within the Bundle, but client systems should have no expectation of such elements being processed by the payer unless prior arrangements have been made. Systems that do not process such elements SHALL ignore unsupported elements unless they are ‘modifier’ elements, in which case the system MAY treat the presence of the element as an error.
Details on how to map the FHIR Bundle to the relevant X12N 278 and 275 messages are expected to be published by ASC X12N. The system is responsible for performing full conversion of all mapped elements, including execution of terminology translations when necessary. In addition, the system SHALL produce an additional 275 message whose binary segment contains a base64-encoded copy of the entire FHIR Bundle resource. This serves two purposes - it provides full audit traceability for the payer and it also allows the payer to directly process the FHIR content, potentially extracting elements not present in the X12 messages if needed. (Note: there is no requirement that payers take any such action.). The 275 BDS01 Filter ID Code element SHALL be set to “B64”. Since the 275 binary segment doesn’t contain a field for the binary data MIME type, any system reading that field will have to parse out the first few characters to determine whether the FHIR resources are encoded using XML or JSON syntax. Translation/mapping systems should be aware that if the size of the attachments as part of a claims submission would exceed the size limitations of a particular recipient, the intermediary should split the attachments into separate 275s to remain within the overall limit. All the data required for an X12N 278 is included in the FHIR Bundle request and response, to stay in compliance with HIPAA transaction requirements.
The mapping of Claim.item is driven by the X12 workflow with the use of identifiers on claim items. Although X12 allows this, the Financial Management workgroup has not seen this in other standards and other jurisdictions. This Implementation Guide uses extensions for the various item identifiers, but should this pattern be found to predominate then this may be promoted to an element in the base resource.
This IG treats everything that happens beyond the defined operations endpoint receiving the FHIR bundle as a black box. This black box includes any business associate(s), clearinghouse(s), payers, contracted review entities, and other intermediaries that may be involved in the PA request and response. It is up to that black box to ensure that any regulatory requirements are met and to perform all processing within the allowed timeframe.
The response to the prior authorization is processed in the reverse order as the request. The system is responsible for converting the ASC X12N 278 response into a FHIR Bundle. The Bundle SHALL start with a ClaimResponse entry that contains information mapped from the 278 response. As well, just like for the prior authorization request, additional Bundle entries must be present for all resources referenced by the ClaimResponse or descendent references. When converting additional Bundle entries, the conversion process SHALL ensure that only one resource is created for a given combination of content. E.g. if the same Practitioner information is referenced in multiple places, only one Practitioner instance should be created - referenced from multiple places as appropriate. When echoing back resources that are the same as were present in the prior authorization request, the system SHALL ensure that the same fullUrl and resource identifiers are used in the response as appeared in the request.
It is possible that the incoming prior authorization Bundle can not be processed due to validation errors or other non-business-errors. In these instances, the receiving system SHALL return OperationOutcome intances that detail why the Bundle could not be processed and no ClaimResponse will be returned. These errors are NOT the errors that are detected by the system processing the request and that can be conveyed in a ClaimResponse via the error capability.
The resulting Bundle is returned as the HTTP body of the POST response.
This is an example of a standard Referral Request / Response sequence between a Primary Care Provider and a Utilization Management Organization. The request example will show how a PCP can request a referral to a specialist for a patient from a UMO. The response example will also show the response.
Joe Smith is a subscriber to Maryland Capital Insurance Company. During a regular physical, Dr. James Gardener, Joe’s primary care physician, diagnoses a potential heart problem. Dr. Gardener determines that it would be best to refer Joe to Dr. Susan Watson, a cardiologist, for a consultation.
Dr. Gardener is required by Maryland Capital Insurance to submit a request for review seeking approval to refer Joe to Dr. Watson.
After review, Maryland Capital approves the referral and responds.
When the ClaimResponse.reviewaction.code is the X12 code for pended, it means that the payer requires additional time to make a final determination on all items within the prior authorization request. In this situation, the client system will need to retrieve the prior authorization response at a later point once a final decision has been made. There are two possible options - polling and subscription. Implementers SHOULD support subscription. Servers SHALL support polling in situations where either party is unable to use the subscription approach.
Note: There are use-cases for multiple systems potentially needing to check on the status of a pended prior authorization. In addition to the provider who submitted the prior authorization request, the status might also be of interest to:
As a result, queries seeking the status of the prior authorization response may come from multiple systems. Servers SHALL permit access to the prior authorization response to systems other than the original submitter. They SHALL require a match on the patient member or subscriber id (identifier on the Claim.patient).
We recognize that knowledge of the Patient member or subscriber identifier may not be sufficient access-control for subsquent queries. We are looking for implementer feedback on this, in particular, on how to pass information through the X12 inquiry mechanism to the payer that help attest to the ‘right to know’.
In this approach, the Client regularly queries the Server to see if the status of the prior authorization has changed. This is done by performing a prior authorization inquiry operation.
Clients SHALL perform this operation in an automated/background manner no more than every 5 minutes for the first 30 minutes and and no more frequently than once every hour after that. They SHOULD perform this query at least once every 12 hours. Clients SHALL support manual invocation of the query by users. There are no constraints on frequency of manual queries.
The project is seeking feedback on whether these maximum frequency requirements are acceptable.
The intermediary SHOULD execute a 278i to return the status. However, if the payer does not support that function, the intermediary SHALL return the most recent copy of the prior authorization response as received from the payer.
Notes:
There is ongoing work on the Subscription resource and it is currently undergoing change such that implementers who are considering using Subscriptions should consult the latest FHIR build material and ask on Zulip for guidance on how to correctly implement Subscriptions.
Subscriptions require more sophistication than polling, but reduce communication overhead by ensuring that queries only occur when data has changed. When using the subscription retrieval mechanism, the Client will POST a new Subscription instance to the Server’s [base]/Subscription endpoint. The Subscription.criteria SHALL be of the form: “identifier=[authorizationresponseid]&patient.identifier=[patientid]&status=active”. (Order of parameters with the search does not matter.)
Once the subscription has been created, the Server SHALL send a notification over the requested channel indicating that the prior authorization response has changed. This may happen when the response is complete, but may also occur when information on one or more of the items has been adjusted but the overall response remains as ‘pended’.
Upon receiving a notification, the Client SHALL - when convenient - execute the same query as shown above in the polling section.
If the retrieved ClaimResponse has an outcome of ‘complete’ or ‘error’, the Client SHALL perform a DELETE on the Subscription.
Systems other than the requesting system may choose not to poll or subscribe to the prior authorization response but instead to check the status at the request of a user. This query is performed in the same manner as the polling query. There are no retry limits for user-initiated status checks.
In some cases, the needs associated with a prior authorization may change after the prior authorization request was submitted. This might be a change to one of the services needed, the timeframe over which the service is provided, the quantity of the service or product, or even the elimination of the need for a given service.
There are four types of changes possible:
In the first case, the Bundle is resubmitted using the $submit operation with the status code changed to ‘cancelled’. In all other cases, the change is requested by creating a new Bundle containing a new Claim resource with its own unique Claim.identifier and posting it using the $submit operation. That resource will point to the previous Claim using the Claim.related element. The relationship type will be ‘replaces’. The new claim resource instance will comply with the Revised Prior Authorization profile.
From an X12 perspective, only those items/attachments that are being added/cancelled/revised need to be present. From an HL7 perspective, resources are generally represented as a cohesive whole, not a set of deltas from a previous resource. This standard therefore provides two different mechanisms for representing the revised prior authorization request:
In this case, the prior authorization request is handled in a typical FHIR manner and all items and supporting information is included in the Bundle - including items that have not changed at all. Changed information is flagged as follows:
The intermediary will create 278 and/or 275 submissions that instantiate the changes (by looking for those items and supportingInfo elements) and will ignore the unchanged items.
The benefit of this approach is that it is consistent with the way the prior authorization would need to be passed around if ever shared in a RESTful manner. However, it can be bandwidth intensive if the prior authorization contains a large number of items, but only a small number of those have changed.
An example of a changed full request can be found at Updated Homecare Request along with the original Homecare Request.
In this case, only the Claim, related resources needed to support the Claim (e.g. submitting organization) and those items and supportingInfo elements that have actually been changed/added are included. I.e. The Claim resource instance doesn’t represent the full prior authorization request, but only the overall prior authorization metadata and the subset of elements that are different. The submitted Bundle will be identical to that above, however it will omit all items that do not have a changed extension. It will also exclude any resources in the Bundle that are no longer needed because the references to them have been removed with the removal of the non-changed Claim.item and/or Claim.supportingInfo elements.
Note that if the change is to cancel the entire request, in the differential approach, there is no need to send any items or supporting Info.
Because this Claim resource instance doesn’t represent the ‘full’ authorization request, but only a subset, the Claim resource instance SHALL also declare a security tag with a value of SUBSETTED to make clear that the resource is incomplete.
An example of a differential request for the same Homecare Request scenario can be found at Differential Homecare Request.
Just as the submission of a changed prior authorization request can be submitted in two different modes, a payer can choose to respond in two different modes. Some payers may include responses for all items in the authorization. Others might only include responses for those items that were specifically changed. (In theory, some payers could also return the items that were changed as well as those that are still pended and thus considered ‘open’.) As for the request, if a ClaimResponse does not contain items corresponding to all that are part of the revised prior authorization (including those cancelled or unmodified), it SHALL declare a security tag with a value of SUBSETTED to make clear that the resource is incomplete.
The intermediary would populate the ClaimResponse Bundle based on the approach the payer had chosen in their 278 response.
NOTE: When querying for the current status of a prior authorization, the prior authorization response SHALL include all items, even if the identifier queried against corresponds to a prior authorization response whose synchronous response was a differential. For example, if a prior authorization revision was submitted changing one item out of four, the synchronous prior authorization response might only contain one item (and a subsetted flag). However, a subsequent query for the status of that prior authorization would always return a prior authorization resource that contained all four items.
PAS systems SHALL ensure that prior authorizations that were initially pended remain available for query for at least 6 months after the anticipated completion of the services whose authorization was requested.
If the prior authorization response is a refusal, it is not permitted to send an ‘update’ to the request in the hopes of receiving a different answer. Instead, a new request must be initiated.
Note that data submitted by client systems will comply with US Core profiles, meaning that codes for medications, conditions, etc. will be those used for clinical purposes, not billing. The intermediary will be responsible for performing any necessary mappings (e.g. SNOMED diagnosis codes to ICD10)
The profiles in this IG are defined to ensure sufficient information to properly populate the X12 specifications, though they also allow for additional data to be present. As well, the data elements in the X12 specifications are allowed to be omitted - what data is required by the payer to process a prior authorization is context and business-rule-specific. Implementers submitting prior authorization requests using PAS must be aware of (and adhere to) their responsibilities with respect to data sharing imposed by regulations such as HIPAA’s “minimum necessary” rule, patient consent rules, etc. This may involve allowing providers to review information prior to data transmission to the payer. Implementations SHALL permit provider review of data prior to transmission, but SHALL NOT require such review.
The sharing of information from provider to payer for determining prior authorization is subject to HIPAA’s “minimum necessary” regulations (specifically 45 CFR 164.514(d)(3) and (d)(4)). Payers are responsible for ensuring that only information necessary to make the prior authorization decision is solicited and providers are responsible for ensuring that only data that is reasonably relevant to the prior authorization decision is transmitted.
Some of the data shared as part of the prior authorization process may have associated constraints on the use of that information for other purposes, including subsequent disclosure to other payers, practitioners, policy-holders, etc. While HL7 FHIR supports conveying this information via security labels on transmitted resources, this information is not currently mappable (and thus findable) in the X12 275 and 278 transactions. Payers who do not view the FHIR version of the transmitted information should be aware of the possibility of these limitations and ensure they have policies that enforce appropriate sharing constraints on data.
In order to access information about a prior authorization, the provider system will need to access the payor system. This will require that the provider system authenticates to the payer system or an intermediary. The specifics of how this authentication are covered is handled within the Da Vinci HRex Implementation guide. PAS Servers SHOULD support server-server OAuth and MAY support mutually authenticated TLS. In a future release of this guide, direction will limit the option to server-server OAuth. Every system implementing the Prior Authorization guide will need to be aware of and follow the guidance in the FHIR Core Specification on Clinical Safety and the Security and Privacy page in the Da Vinci HRex guide.
Once the system authentication has occurred, the payer will perform any authorization required for the provider to see the current state of the prior authorization.
It is the intent of this implementation guide to provide specifications for the exchange of prior authorization in a way that is conducive to developing test scripts and a reference implementation (RI) that can be used to validate/exercise the IG at connectathons and during piloting and production deployment. It is also the intent of this guide that any test scripts will include testing of: