This page is part of the Da Vinci Data Exchange for Quality Measures (DEQM) FHIR IG (v3.0.0: STU 3) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 5.0.0. For a full list of available versions, see the Directory of published versions
As supported in this guide, a gap in care is defined as a discrepancy between standards of care specified in quality measures and the services that were provided. Gaps in care may be identified because no care was provided, or because data about care provided is missing from the system calculating the data.
Actual gaps in care can adversely affect member outcomes, and lack of awareness that care was provided can contribute to unnecessary costs. Identifying, anticipating, and communicating gaps in care between involved actors, at the point of care, is critical for providing opportunities to improve quality of care.
Research has shown that care gaps can be both harmful and costly when they are not properly managed. For example, not managing specific aspects of chronic diseases (e.g., hemoglobin A1C control with respect to diabetes management) can lead to serious complications and escalate healthcare costs. Resolving gaps in care is important to payers, providers, and the patients they serve. Performing care that resolves gaps in care can positively influence patient health and improve quality scores and reimbursement under risk-sharing arrangements. Gaps in care may exist for several reasons. The following are some common scenarios where an actual or potential gap may exist.
A Gaps in Care Report is designed to communicate actual or perceived gaps in care between systems, such as the payer’s system and provider’s EMR. The report provides opportunities for providers to provide missing care and/or to communicate care provision data to payers. The report may also provide information for upcoming care opportunities, prospective gaps.
In Figure 2-12, the red circle represents the Gaps in Care Reporting flow portion of the Quality Improvement Ecosystem. Please see The Quality Improvement Ecosystem Diagram.
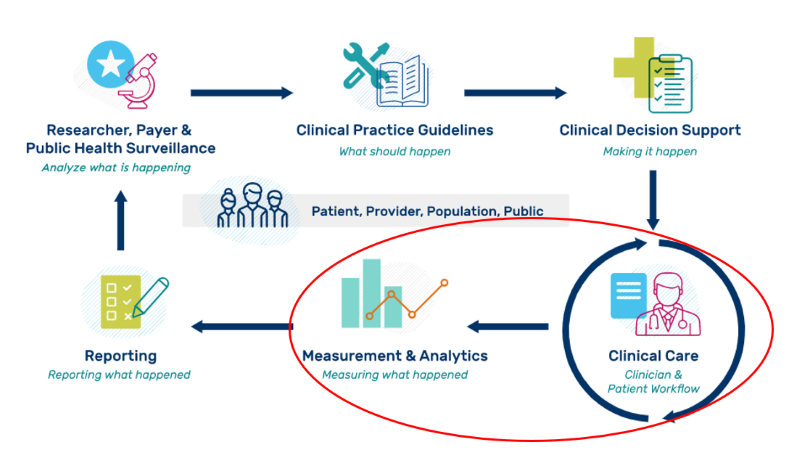
The gaps in care flow is between a provider and a measurement organization’s system performing analytics.
Note that this implementation guide does not address actual workflow around managing the process of requesting a Gaps in Care Report and to whom the report should be sent.
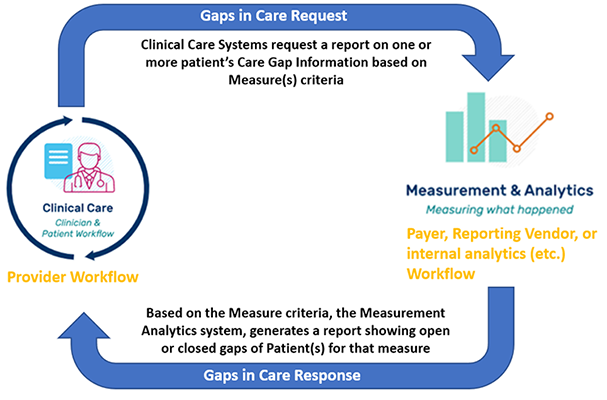
Figure 2-13 reflects the details within the red circle representing the Gaps in Care Reporting flow portion of the Quality Improvement Ecosystem.
The Gaps in Care Reporting uses the DEQM Individual MeasureReport Profile. This allows the Gaps in Care Reporting to use the same machinery as the Individual Reporting to calculate measures and represent the results of individual calculation.
The following resources are used in the Gaps in Care Reporting Scenario:
| Resource Type | Profile Name | Link to Profile |
|---|---|---|
| Bundle | DEQM Gaps In Care Bundle Profile | DEQM Gaps In Care Bundle Profile |
| Composition | DEQM Gaps In Care Composition Profile | DEQM Gaps In Care Composition Profile |
| DetectedIssue | DEQM Gaps In Care DetectedIssue Profile | DEQM Gaps In Care DetectedIssue Profile |
| Group | DEQM Gaps In Care Group Profile | DEQM Gaps In Care Group Profile |
| MeasureReport | DEQM Individual MeasureReport Profile | DEQM Individual MeasureReport Profile |
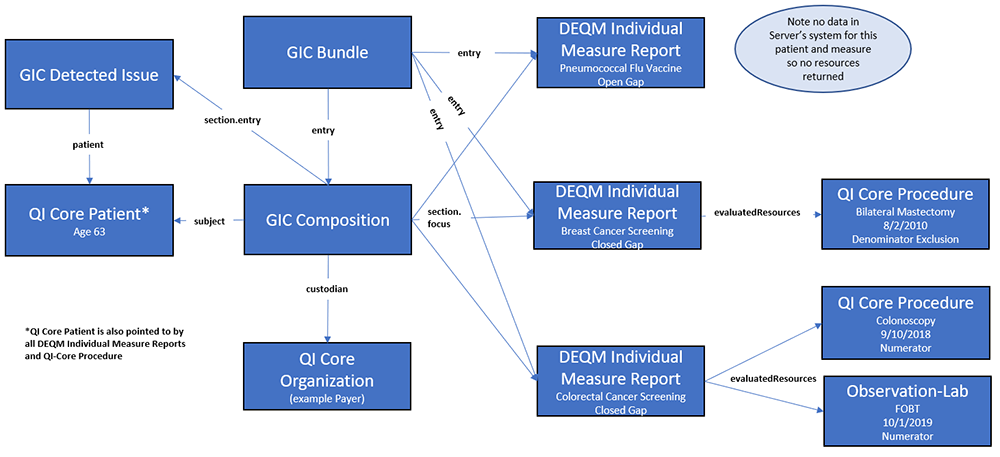
Figure 2-14 provides a graphical view of how these resources are related. A Composition is created for each Patient (linked via subject element) and is contained in a Bundle. The Composition resource references one or more DEQM Individual MeasureReport resources. One MeasureReport for each Measure included in the report. If the generator of the MeasureReport resource has data used in the Measure, they are linked under evaluatedResource element. The DEQM Population Reference Extension on the evaluatedResource documents how that resource contributed to the measure, i.e. numerator, denominator, etc.
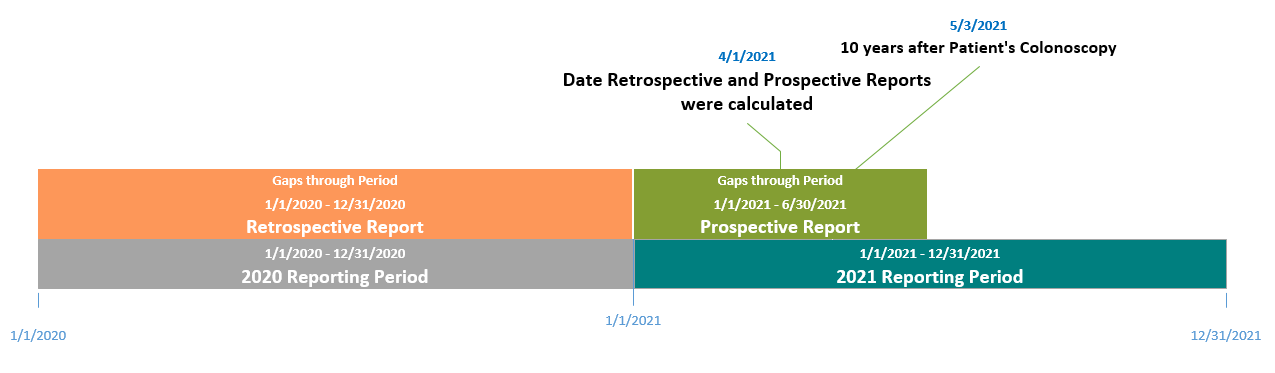
Gaps through period is the time period defined by a Client for running the Gaps in Care Report. When the gaps through period ends on a date that is in the future, the Gaps in Care Reporting is said to look for care gaps prospectively. In this scenario, it provides providers with opportunities to assess anticipated open gaps and take proper actions to close the gaps. When the gaps through period ends on a date that is in the past, the Gaps in Care Reporting is said to look for care gaps retrospectively. In the retrospective scenario, identified open gaps can no longer be acted upon to meet the quality measure. In the example below, Colorectal Cancer Screening (CMS130) with measureId EXM130-7.3.000 is used as an example measure.
| Use Case | care-gaps Operation | Gaps Through Period Start Date | Gaps Through Period End Date | Report Calculated Date | Colorectal Cancer Screening - Colonoscopy Date | Gaps in Care Report |
|---|---|---|---|---|---|---|
| Prospective Use Case | $care-gaps?periodStart=2021-01-01&periodEnd=2021-06-30&subject=Patient/123&measureId=EXM130-7.3.000&status=open-gap | 2021-01-01 | 2021-06-30 | 2021-04-01 | Example: patient had colonoscopy on 2011-05-03 | Returns gaps through 2021-06-30. The Gaps in Care Report indicates the patient has an open gap for the colorectal cancer screening measure. By 2021-06-30, the colonoscopy would be over 10 years. |
| Retrospective Use Case | $care-gaps?periodStart=2020-01-01&periodEnd=2020-12-31&subject=Patient/123&measureId=EXM130-7.3.000&status=open-gap | 2020-01-01 | 2020-12-31 | 2021-04-01 | Example: patient had colonoscopy on 2011-05-03 | Returns gaps through 2020-12-31. The Gaps in Care Report indicates the patient has a closed gap for the colorectal cancer screening measure. Since on 2020-12-31, the procedure would have occurred within the specified 10-year timeframe. |
The timeline below represents the data described above. A colonoscopy procedure per the Colorectal Cancer Screen measure is required every 10 years. If as in the example above, the patient had a colonoscopy done on May 3rd, 2011, another one would be due and the gap opened on May 3rd, 2021.
The care-gaps operation is used to run a Gaps in Care Report. In this guide, we have updated the base care-gaps operation in the R4 Release of the FHIR (FHIR R4) Specification to allow for the specification of additional parameters that will be useful to the communities needing this report. This operation is run on the Measure resource and allows a Server to create a Gaps in Care Report based on the quality measures available in the Server’s system.
A report calculated on any given date provides all of the data from the server’s system as of that date. A request for a previous time period will still show all data available as of the date the report is calculated. Therefore, a requester can ask for multiple reports, save them and compare them, but not request data “as of” previous dates.
The updated operation, care-gaps, makes the following changes to the existing input parameters in the base operation:
Several new input parameters are specified and added to the care-gaps operation defined in this guide:
The care-gaps operation has an out parameter: return. In comparison to the return output parameter specified in the base care-gaps operation, the return here returns a Parameters resource that contains zero or more parameter, with each parameter containing a Bundle resource that conforms to the DEQM Gaps In Care Bundle Profile.
Through the requirement analysis of the Gaps in Care Reporting for the STU3 ballot, it is determined that existing care-gaps operation in FHIR R4 requires a re-design. The plan is to promote the care-gaps operation specified in this version of the guide to the next release of the base FHIR specification.
Figure 2-16 shows an example workflow for running the care-gaps operation against a payer’s system for a single patient.
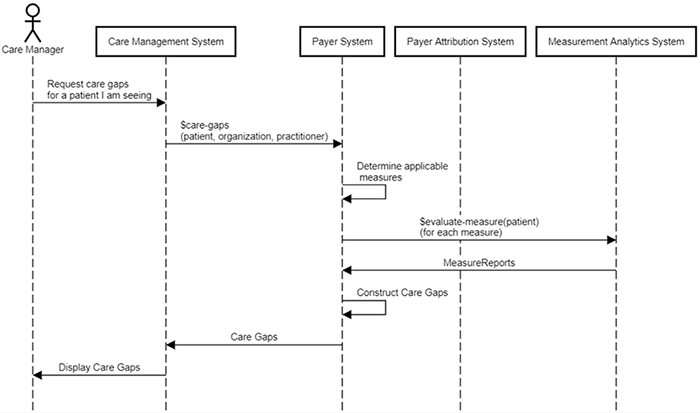
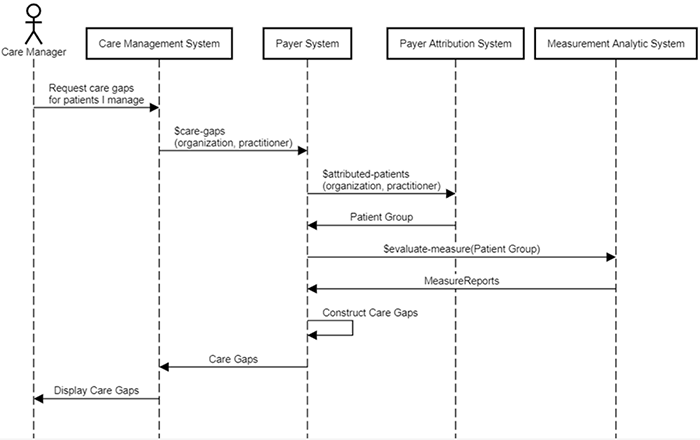
Figure 2-17 shows an example workflow for running the care-gaps operation against a payer’s system for a group of patients.
This section describes the profiles used for Gaps in Care Reporting and how they are used to construct a Gaps in Care Report.
The care-gaps operation returns a Parameters resource that contains zero or more parameter with document bundle for each patient for which a Gaps in Care report is calculated. The bundle SHALL conform to the DEQM Gaps In Care Bundle Profile. A Gaps In Care Bundle SHALL contain a Composition entry, which uses the DEQM Gaps In Care Composition Profile.
The DEQM Gaps in Care Composition Profile builds on the base FHIR Composition resource, where its type code is constrained to a fixed LOINC code to identify the Composition as a Gaps in Care Report. The subject of a Gaps In Care Composition is required, it is used to reference the patient, QI Core Patient, the Gaps in Care Report is for. The Gaps In Care Composition SHALL contain one to many section(s). Each section has a focus element that references an Individual MeasureReport for a specific measure. All Individual MeasureReport referenced SHALL be for the same patient specified in the Composition subject. Each section SHALL also contain one or more entry of DetectedIssue using the DEQM Gaps In Care DetectedIssue Profile for the measure regardless of its gap status (e.g., open or closed).
The Individual MeasureReport SHALL conform to the DEQM Individual MeasureReport Profile. This profile contains an optional extension, DEQM Population Reference Extension, on the evaluatedResource element. This extension allows the Server to indicate how an evaluatedResource, such as a colonoscopy procedure, was used to produce the measure calculation results by linking it to a specific population criteria identified by the population criteria id that equals to Measure.population.group.id. If an evaluatedResource contributes to multiple population criteria such as denominator and numerator, this can be represented by having two population reference extensions. One extension has value that references the denominator population criteria id and the other extension has value that references the numerator population criteria id.
The DEQM Gaps In Care DetectedIssue Profile has a fixed code CAREGAP indicating the detected issue is in the Care Gaps detected issue category. Each DetectedIssue SHALL contain at least one evidence element that each evidence SHALL provide a detail that references either a DEQM Individual MeasureReport of the measure or a GuidanceResponse.
The DEQM Gaps in Care Composition Profile may also contain all supporting resources referenced by the Composition and its contained measure reports. As with other compositions, this resource can contain a narrative which can be displayed as a textual report.
The date element of the MeasureReport resource contains the date the open/closed gap was calculated.
Member attribution establishes associations between providers and payers. The process of establishing and exchanging member lists for Gaps in Care Reports is not in the scope of the DEQM IG. One possible way of exchanging Member Attribution Lists between providers and payers is described in the Da Vinci - Risk Based Contracts Member Attribution (ATR) List IG.
GET|[base]
Scenario:
A Client would like to know if the patient, gaps-patient01, has any open or closed gaps for the colorectal cancer screening measure and the cervical cancer screening measure for the period from 2020-01-01 to 2020-12-31. The Client requested a Gaps in Care Report from a Server’s system on 2020-06-30.
GET Gaps in Care Report
GET [base]/Measure/$care-gaps?measureurl=http://hl7.org/fhir/us/davinci-deqm/Measure/measure-exm130-example|2.0.0&measureurl=http://hl7.org/fhir/us/davinci-deqm/Measure/measure-exm124-example|2.0.0&subject=Patient/gaps-patient01&periodStart=2020-01-01&periodEnd=2020-12-31&status=open-gap&status=closed-gap
Request body
(Note that request body is not applicable in this example)
Response
HTTP/1.1 200
Date: Wed, 22 July 2020 01:02:06 GMT
Content-Type: application/fhir+json;charset=UTF-8
...Other Headers...
{
"resourceType": "Bundle",
"id": "single-gaps-open-indv-report01",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/gaps-bundle-deqm"
]
},
"identifier": {
"system": "urn:ietf:rfc:3986",
"value": "urn:uuid:77f43ef5-8c60-4222-ae58-36969063a093"
},
"type": "document",
"timestamp": "2020-06-30T13:08:53+00:00",
"entry": [
{
"fullUrl": "http://example.org/fhir/gaps/Composition/gaps-composition01",
"resource": {
"resourceType": "Composition",
"id": "gaps-composition01",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/gaps-composition-deqm"
]
},
"status": "final",
"type": {
"coding": [
{
"system": "http://loinc.org",
"code": "96315-7",
"display": "Gaps in care report"
}
]
},
"subject": {
"reference": "Patient/gaps-patient01"
},
"date": "2020-06-30T13:08:53+00:00",
"author": [
{
"reference": "Organization/gaps-organization-reportingvendor"
}
],
"title": "Care Gap Report for patient gaps-patient01",
"section": [
{
"title": "Colorectal Cancer Screening",
"focus": {
"reference": "MeasureReport/gaps-indv-measurereport01"
},
"entry": [
{
"reference": "DetectedIssue/gaps-detectedissue01"
}
]
},
{
"title": "Cervical Cancer Screening",
"focus": {
"reference": "MeasureReport/gaps-indv-measurereport02"
},
"entry": [
{
"reference": "DetectedIssue/gaps-detectedissue02"
}
]
}
]
}
},
{
"fullUrl": "http://example.org/fhir/gaps/MeasureReport/gaps-indv-measurereport01",
"resource": {
"resourceType": "MeasureReport",
"id": "gaps-indv-measurereport01",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/indv-measurereport-deqm"
]
},
"extension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-measureScoring",
"valueCodeableConcept": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-scoring",
"code": "proportion"
}
]
}
},
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-certificationIdentifier",
"valueIdentifier": {
"system": "urn:oid:2.16.840.1.113883.3.2074.1",
"value": "0015HQN9BD3304E"
}
},
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-reportingVendor",
"valueReference": {
"reference": "Organization/gaps-organization-reportingvendor"
}
}
],
"status": "complete",
"type": "individual",
"measure": "http://hl7.org/fhir/us/davinci-deqm/Measure/measure-exm130-example",
"subject": {
"reference": "Patient/gaps-patient01"
},
"date": "2020-06-30T13:08:52+00:00",
"reporter": {
"reference": "Organization/organization01"
},
"period": {
"start": "2020-01-01T00:00:00+00:00",
"end": "2020-12-31T00:00:00+00:00"
},
"improvementNotation": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-improvement-notation",
"code": "increase"
}
]
},
"group": [
{
"id": "group-exm130",
"population": [
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "initial-population",
"display": "Initial Population"
}
]
},
"count": 1
},
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "numerator",
"display": "Numerator"
}
]
},
"count": 0
},
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "denominator",
"display": "Denominator"
}
]
},
"count": 1
},
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "denominator-exclusion",
"display": "Denominator Exclusion"
}
]
},
"count": 0
}
],
"measureScore": {
"value": 0.0
}
}
],
"evaluatedResource": [
{
"extension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-populationReference",
"valueString": "initial-population"
}
],
"reference": "Encounter/gaps-encounter01"
},
{
"extension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-populationReference",
"valueString": "initial-population"
}
],
"reference": "Patient/gaps-patient01"
}
]
}
},
{
"fullUrl": "http://example.org/fhir/gaps/MeasureReport/gaps-indv-measurereport02",
"resource": {
"resourceType": "MeasureReport",
"id": "gaps-indv-measurereport02",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/indv-measurereport-deqm"
]
},
"extension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-measureScoring",
"valueCodeableConcept": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-scoring",
"code": "proportion"
}
]
}
},
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-certificationIdentifier",
"valueIdentifier": {
"system": "urn:oid:2.16.840.1.113883.3.2074.1",
"value": "0015HQN9BD3304E"
}
},
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-reportingVendor",
"valueReference": {
"reference": "Organization/gaps-organization-reportingvendor"
}
}
],
"status": "complete",
"type": "individual",
"measure": "http://hl7.org/fhir/us/davinci-deqm/Measure/measure-exm124-example",
"subject": {
"reference": "Patient/gaps-patient01"
},
"date": "2020-07-02T13:08:52+00:00",
"reporter": {
"reference": "Organization/organization01"
},
"period": {
"start": "2020-01-01T00:00:00+00:00",
"end": "2020-12-31T00:00:00+00:00"
},
"improvementNotation": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-improvement-notation",
"code": "increase"
}
]
},
"group": [
{
"id": "group-exm124",
"population": [
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "initial-population",
"display": "Initial Population"
}
]
},
"count": 1
},
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "numerator",
"display": "Numerator"
}
]
},
"count": 0
},
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "denominator",
"display": "Denominator"
}
]
},
"count": 1
},
{
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/measure-population",
"code": "denominator-exclusion",
"display": "Denominator Exclusion"
}
]
},
"count": 0
}
],
"measureScore": {
"value": 0.0
}
}
],
"evaluatedResource": [
{
"extension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-populationReference",
"valueString": "initial-population"
},
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-populationReference",
"valueString": "denominator"
}
],
"reference": "Encounter/gaps-encounter01"
},
{
"extension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-populationReference",
"valueString": "initial-population"
},
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-populationReference",
"valueString": "denominator"
}
],
"reference": "Patient/gaps-patient01"
}
]
}
},
{
"fullUrl": "http://example.org/fhir/gaps/DetectedIssue/gaps-detectedissue01",
"resource": {
"resourceType": "DetectedIssue",
"id": "gaps-detectedissue01",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/gaps-detectedissue-deqm"
]
},
"modifierExtension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-gapStatus",
"valueCodeableConcept": {
"coding": [
{
"system": "http://hl7.org/fhir/us/davinci-deqm/CodeSystem/gaps-status",
"code": "closed-gap"
}
]
}
}
],
"status": "final",
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/v3-ActCode",
"code": "CAREGAP",
"display": "Care Gaps"
}
]
},
"patient": {
"reference": "Patient/gaps-patient01"
},
"evidence": [
{
"detail": [
{
"reference": "MeasureReport/gaps-indv-measurereport01"
}
]
}
]
}
},
{
"fullUrl": "http://example.org/fhir/gaps/DetectedIssue/gaps-detectedissue02",
"resource": {
"resourceType": "DetectedIssue",
"id": "gaps-detectedissue02",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/gaps-detectedissue-deqm"
]
},
"modifierExtension": [
{
"url": "http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/extension-gapStatus",
"valueCodeableConcept": {
"coding": [
{
"system": "http://hl7.org/fhir/us/davinci-deqm/CodeSystem/gaps-status",
"code": "closed-gap"
}
]
}
}
],
"status": "final",
"code": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/v3-ActCode",
"code": "CAREGAP",
"display": "Care Gaps"
}
]
},
"patient": {
"reference": "Patient/gaps-patient01"
},
"evidence": [
{
"detail": [
{
"reference": "MeasureReport/gaps-indv-measurereport02"
}
]
}
]
}
},
{
"fullUrl": "http://example.org/fhir/gaps/Encounter/gaps-encounter01",
"resource": {
"resourceType": "Encounter",
"id": "gaps-encounter01",
"meta": {
"profile": [
"http://hl7.org/fhir/us/core/StructureDefinition/us-core-encounter"
]
},
"status": "finished",
"class": {
"system": "http://terminology.hl7.org/CodeSystem/v3-ActCode",
"code": "AMB",
"display": "ambulatory"
},
"type": [
{
"coding": [
{
"system": "http://www.ama-assn.org/go/cpt",
"code": "99201",
"display": "Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A problem focused history; A problem focused examination; Straightforward medical decision making. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient's and/or family's needs. Usually, the presenting problem(s) are self limited or minor. Typically, 10 minutes are spent face-to-face with the patient and/or family."
}
]
}
],
"subject": {
"reference": "Patient/gaps-patient01"
},
"period": {
"start": "2020-05-30T00:00:00-00:00",
"end": "2020-05-31T00:00:00-00:00"
}
}
},
{
"fullUrl": "http://example.org/fhir/gaps/Patient/gaps-patient01",
"resource": {
"resourceType": "Patient",
"id": "gaps-patient01",
"meta": {
"profile": [
"http://hl7.org/fhir/us/core/StructureDefinition/us-core-patient"
]
},
"extension": [
{
"extension": [
{
"url": "ombCategory",
"valueCoding": {
"system": "urn:oid:2.16.840.1.113883.6.238",
"code": "2028-9",
"display": "Asian"
}
},
{
"url": "text",
"valueString": "Asian"
}
],
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-race"
},
{
"extension": [
{
"url": "ombCategory",
"valueCoding": {
"system": "urn:oid:2.16.840.1.113883.6.238",
"code": "2135-2",
"display": "Hispanic or Latino"
}
},
{
"url": "text",
"valueString": "Hispanic or Latino"
}
],
"url": "http://hl7.org/fhir/us/core/StructureDefinition/us-core-ethnicity"
}
],
"identifier": [
{
"use": "usual",
"type": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/v2-0203",
"code": "MR",
"display": "Medical Record Number"
}
]
},
"system": "http://hospital.smarthealthit.org",
"value": "999995992"
}
],
"name": [
{
"family": "Susan",
"given": [
"Parker"
]
}
],
"gender": "female",
"birthDate": "1965-01-01"
}
},
{
"fullUrl": "http://example.org/fhir/gaps/Organization/gaps-organization-reportingvendor",
"resource": {
"resourceType": "Organization",
"id": "gaps-organization-reportingvendor",
"meta": {
"profile": [
"http://hl7.org/fhir/us/davinci-deqm/StructureDefinition/organization-deqm"
]
},
"identifier": [
{
"use": "official",
"type": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/v2-0203",
"code": "TAX",
"display": "Tax ID number"
}
]
},
"system": "urn:oid:2.16.840.1.113883.4.4",
"value": "123446789",
"assigner": {
"display": "www.irs.gov"
}
}
],
"active": true,
"type": [
{
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/organization-type",
"code": "pay",
"display": "Payer"
}
]
}
],
"name": "GapsReportingVendor01",
"telecom": [
{
"system": "phone",
"value": "(+1) 401-545-1212"
}
],
"address": [
{
"line": [
"13 Drive Street"
],
"city": "Cityplace",
"state": "MA",
"postalCode": "01101",
"country": "USA"
}
]
}
}
]
}
If Clients are requesting Gaps in Care Reports for many patients/members, they may consider using the FHIR Asynchronous Request Patterns for the Bulk Data exchange operation.
GET|[base]
Scenario:
The Client would like to request Gaps in Care Reports on many patients. They have created a FHIR Group Resource using the DEQM Gaps In Care Group Profile with the id of 123. Because they expect the creation of the reports to take a while and many FHIR bundles will be returned and be processed, they would like to make the request in an asynchronous manner returning NDJSON that will be easier for them to process.
The request below asks for Group id of 123 to be run asynchronously with FHIR+ndjson as the output format. The header portions should be entered in the API client header section. For example, in the Postman tool, enter “Prefer” in Key and “respond-async” in Value as an entry in the Headers tab.
GET Gaps in Care Report Using Bulk Data
Run $care-gaps operation in an asynchronous mode:
GET [base]/Measure/$care-gaps?measureurl=http://hl7.org/fhir/us/davinci-deqm/Measure/measure-exm130-example|2.0.0&subject=Group/123&periodStart=2020-01-01&periodEnd=2020-12-31&status=open-gap&status=closed-gap&_outputFormat=application/fhir+ndjson
Headers:
Prefer respond-asyncAccept application/fhir+jsonNote that both Prefer and Accept are required. Prefer specifies the response is immediate or asynchronous, which SHALL be set to respond-async. Accept specifies the format of the optional OperationOutcome response to the kick-off request. Any of the Serialization Format Representations are supported. See the base FHIR specification Asynchronous Request Patterns for details.
Query Parameters:
_outputFormat (string, optional, defaults to application/fhir+ndjson)Currently, only application/fhir+ndjson is supported.