This page is part of the Consumer Real-time Pharmacy Benefit Check (v0.1.0: STU 1 Ballot 1) based on FHIR R4. The current version which supercedes this version is 1.0.0. For a full list of available versions, see the Directory of published versions 
Example RTPBC response scenario using FHIR messaging
In this example:
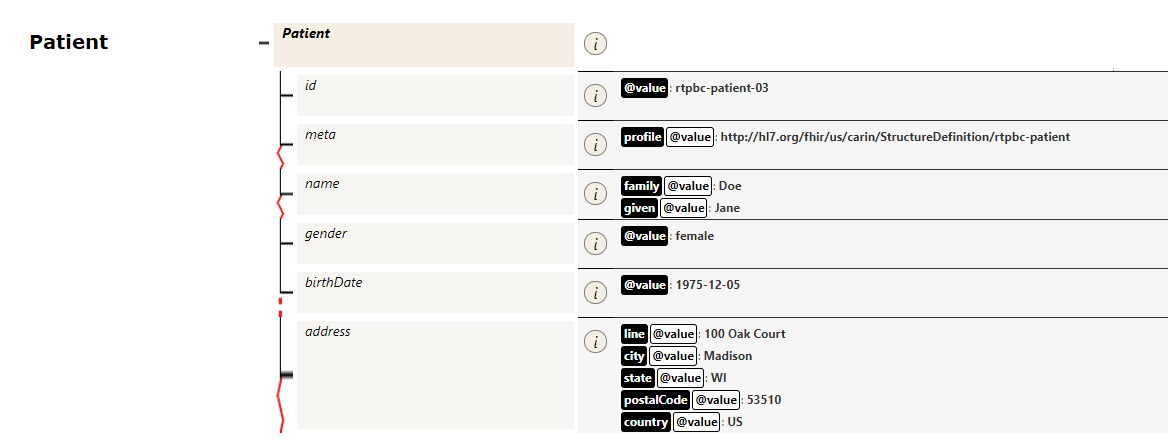
- the client is a patient application
- the server is the patient’s insurer (specifically, the party that manages the patient’s pharmacy benefit)
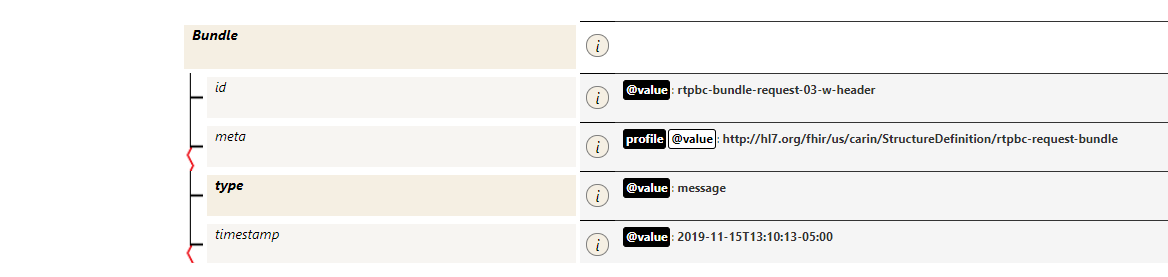
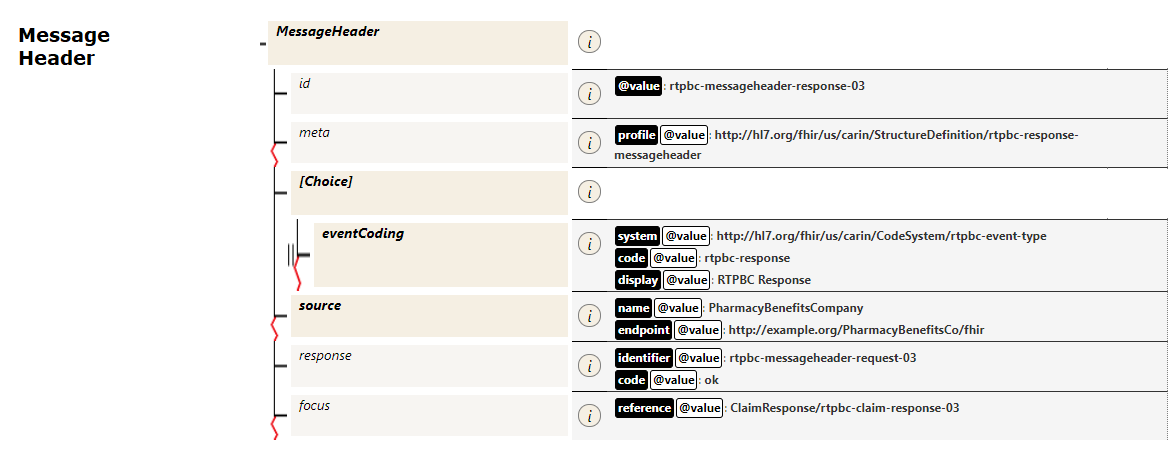
- the response is returned as a Bundle containing a ClaimResponse and supporting resources, in response to a Claim.$submit operation
Content:
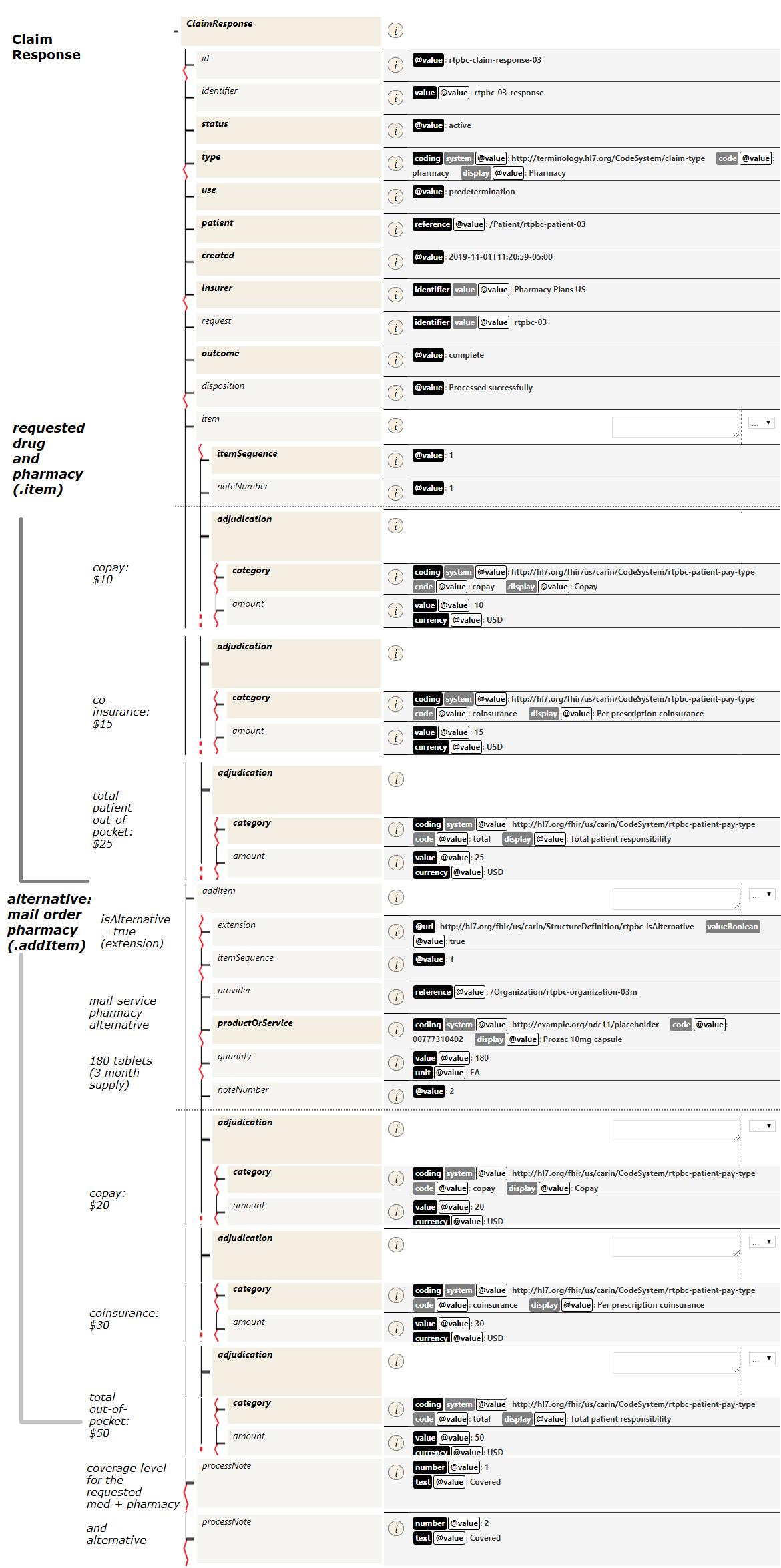
- the requested medication is Prozac 10mg capsule, 60 capsules, and the requested pharmacy is Hometown Drug. Adjudication returned in the ClaimResponse.item composite
- the .item contains patient costs for the requested drug and pharmacy combination
- the .addItem composite holds an alternative fulfillment (the requested drug at a different pharmacy). Adjudication is returned in the ClaimResponse.addItem composite
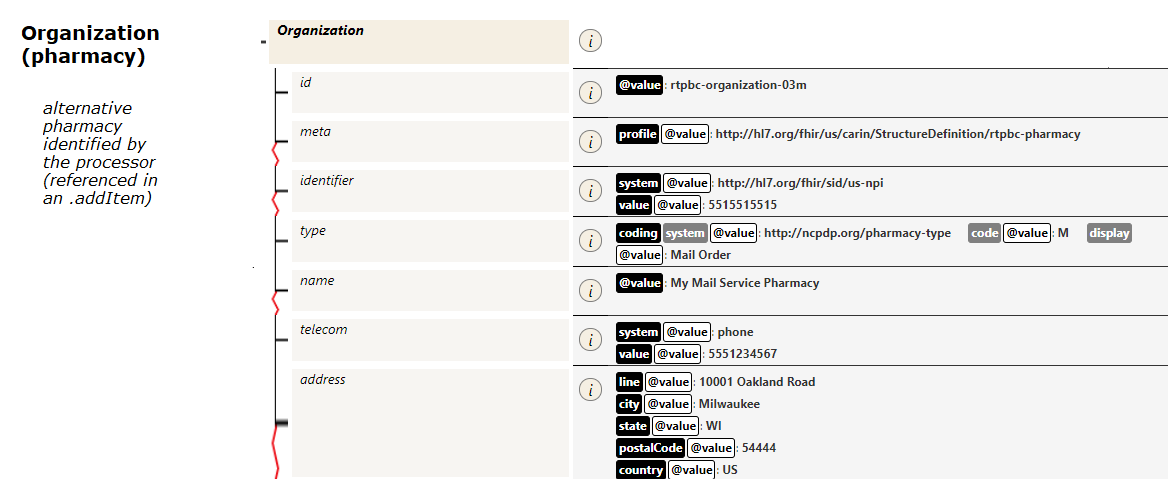
- a pharmacy Organization resource describes the alternative pharmacy option identified by the processor
- summary coverage information (e.g., Covered, Covered but requiring PA) is returned in the .processNote element - linked to the particular item using the processNote.number field