This page is part of the Consumer Real-time Pharmacy Benefit Check (v1.0.0: STU 1) based on FHIR R4. This is the current published version. For a full list of available versions, see the Directory of published versions 
Format(s):
In this example:
Content:
Narrative view
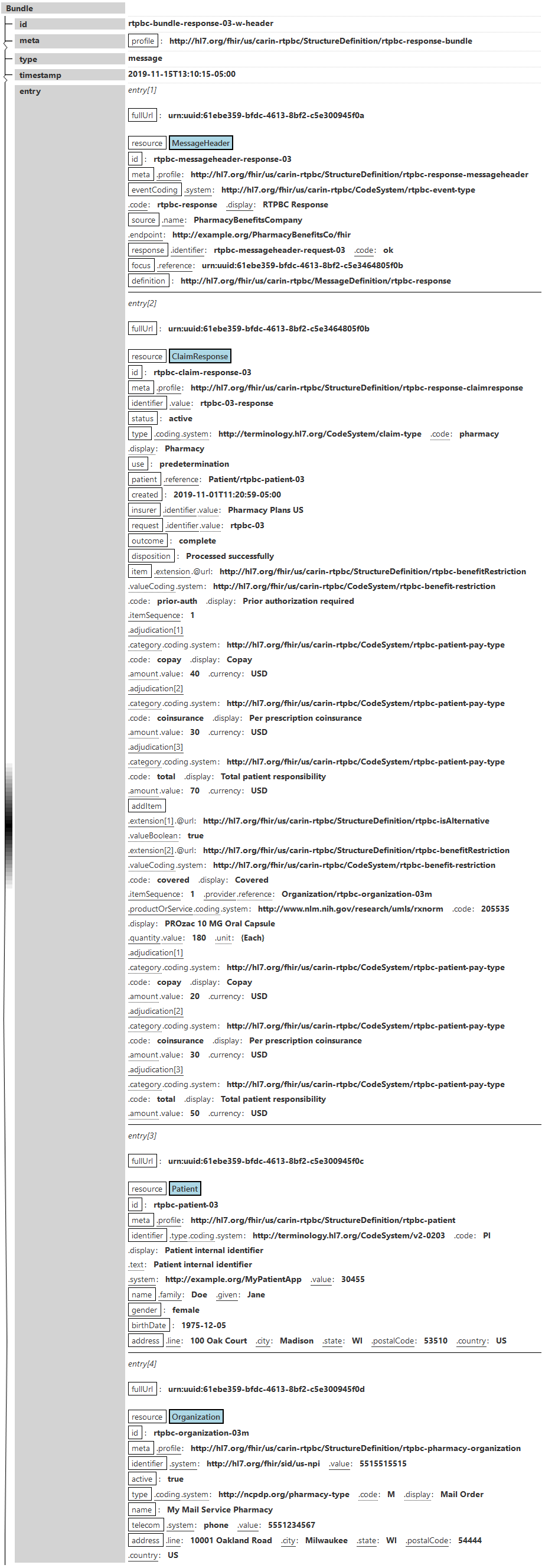
Bundle rtpbc-bundle-response-03-w-header of type message
Entry 1 - Full URL = urn:uuid:61ebe359-bfdc-4613-8bf2-c5e300945f0a
Resource MessageHeader:
Entry 2 - Full URL = urn:uuid:61ebe359-bfdc-4613-8bf2-c5e3464805f0b
Resource ClaimResponse:
Entry 3 - Full URL = urn:uuid:61ebe359-bfdc-4613-8bf2-c5e300945f0c
Resource Patient:
Entry 4 - Full URL = urn:uuid:61ebe359-bfdc-4613-8bf2-c5e300945f0d
Resource Organization: