This page is part of the Consumer Real-time Pharmacy Benefit Check (v1.0.0: STU 1) based on FHIR R4. This is the current published version. For a full list of available versions, see the Directory of published versions 
Use Cases
Goal
The goal of the consumer-focused real-time pharmacy benefit check (consumer RTPBC) is to inform a patient of the cost and insurance coverage related to medications they’ve been prescribed. This involves two key aspects:
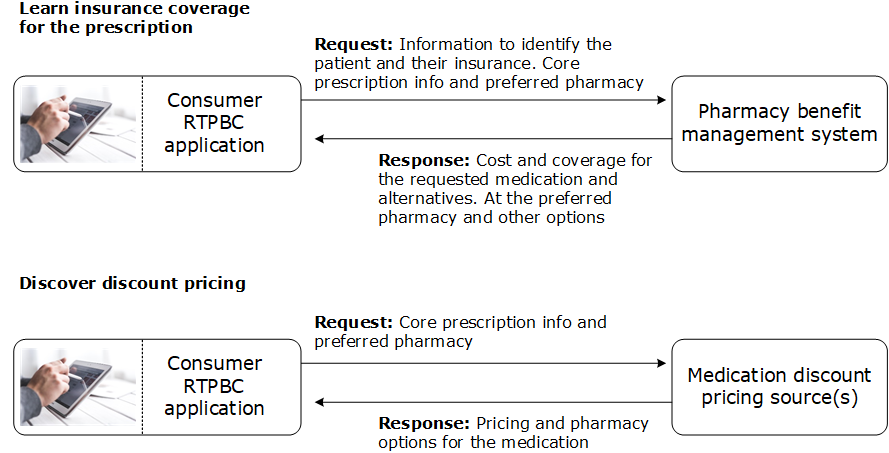
- Use case 1: Enable the patient to find out how their medications will be covered by their insurance, including out of pocket costs and any coverage restrictions or requirements that might apply
- Use case 2: Help the patient discover discount pricing available for the medication.
Usage context
The real-time pharmacy benefit check is designed to provide accurate cost information based on the specifics of a patient prescription. Details such as the specific drug name, dose form, strength and quantity must match the prescription exactly in order to receive reliable results.
However, a patient may wish to use the process for a medication they haven’t yet been prescribed, for example to understand its cost compared to their current treatment. In that circumstance, the results must be viewed as approximate information that may not reflect their actual cost when their prescriber has ordered a particular product and dosage
Use case flows
At a high level, the process looks like this…
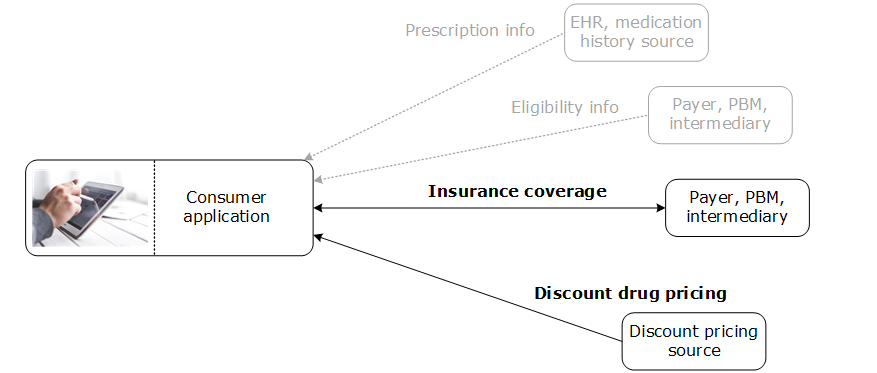
Participants
- the patient, who wishes to understand how their medication is covered by their insurance: their out of pocket cost, restrictions, and pharmacy options. Using the gathered information, the patient can learn whether the drug is covered, compare insurance out of pocket costs between pharmacies–and can also compare to cash prices and discount options gathered by their app
- the consumer app that submits the RTPBC request to the payer, and interprets the response for the patient
- the patient’s insurer or agent that processes the RTPBC request and returns a response containing pricing, coverage restrictions, pharmacy options for the requested drug and alternative medications (typically the pharmacy benefit manager that handles the patient’s prescription benefit)
- a medication pricing information source
Consumer App Responsibilities
- the patient’s app gathers information about the prescription… entered by the patient or imported from another source
- the patient provides coverage information from their insurance card, or the app retrieves it using an eligibility service (outside the scope of this guide)
- the app packages up the patient, coverage, prescription and preferred pharmacy information in HL7 FHIR® resources and submits them to the patient’s insurer
- the app interprets and presents the returned information in an understandable way, possibly presenting insurance coverage alongside cash or discount pricing gathered from other sources
Insurer Responsibilities
- determines the patient cost and coverage details for the requested pharmacy and potentially for other pharmacy options–such as a mail service pharmacy
- also checks for preferred alternative medications with better coverage under the patient’s plan, and returns cost, coverage and pharmacy options for those as well
Medication Pricing Source Responsibilities
- determines the price for the requested medication and pharmacy combination and other medication/pharmacy options
- identifies discounts that apply, related to coupons or memberships
If the insurer or medication pricing source cannot complete processing of the request, it returns information about the exception that occurred. See the Error Handling page
The patient’s app might gather related information (e.g., medication information or insurance eligibility) before submitting the consumer RTPBC request.
These exchanges are outside the scope of this guide.
Next Page