This page is part of the Situational Awareness for Novel Epidemic Response (v1.0.0: STU 1) based on FHIR R4. This is the current published version in its permanent home (it will always be available at this URL). For a full list of available versions, see the Directory of published versions 
This section of the implementation guide walks through an example for automating computation of a measure.
The definitions for these proposed groupings appear below. For simplicity and brevity, the definitions below are provided in a slightly modified version of the FHIR Shorthand notation. The modification introduces “with fieldparts do” keyword to shorten repetitions.
For example:
* with name do
** given[] = "Robert"
** given[] = "Rob"
** last = "Williams"
Would be the same as
* name.given[0] = "Robert"
* name.given[1] = "Rob"
* name.last = "Williams"
FHIRPath Expressions used for this measure will use the functions defined by FluentQuery defined in Appendix B of this guide to make the expressions more readable.
NOTE: The completed measure may vary slightly from the text in this section.
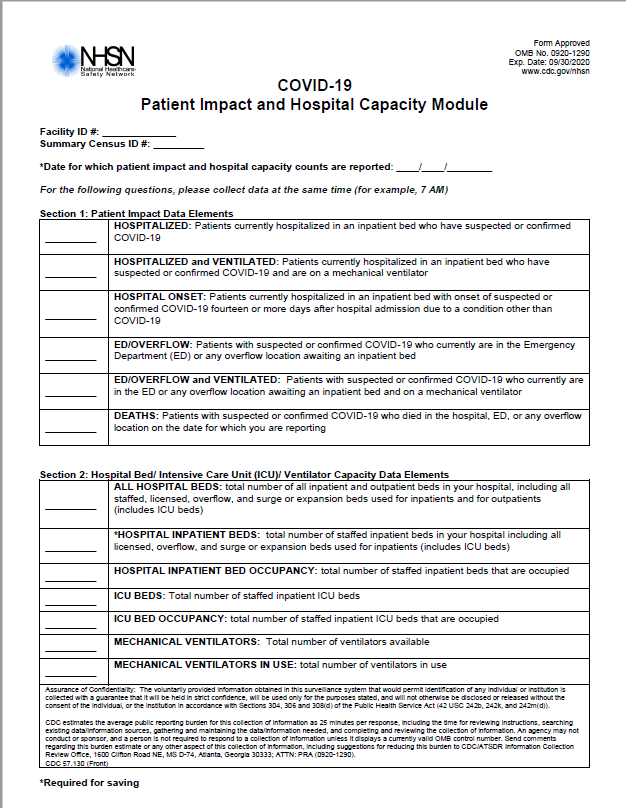
Like the phrase book, this walkthrough is based on the measure derived from the CDC Patient Impact and Hospital Capacity module shown below. This measure example is provided for the purposes of discussion, it is neither an official CDC publication nor a normative artifact in this guide.
The top part of the measure contains the metadata describing the measure itself, giving it a name, an identifier, author and publisher, et cetera. These components are described in more detail below.
The measure begins by describing the author and providing contact information using an e-mail address. This enables those with access to the measure content to easily contact the organization which authored it.
* author.name = "Centers for Disease Control/National Healthcare Safety Network (CDC/NHSN)"
* author.telecom.system = #email
* author.telecom.value = "mailto:nhsn@cdc.gov"
This measure should be reported daily. This makes uses of the ReportingPeriod extension and the MeasureReportingTiming profile to identify how often to report the measure.
* extension[measureTiming].valueTiming.repeat.frequency = 1
* extension[measureTiming].valueTiming.repeat.period = 1
* extension[measureTiming].valueTiming.repeat.periodUnit = http://unitsofmeasure.org#d "day"
Each measure has both a human readable title, and computation oriented name, and a URL which uniquely identifies it.
* name = "ComputableCDCPatientImpactAndHospitalCapacity"
* url = "http://hl7.org/fhir/uv/saner/Measure/ComputableCDCPatientImpactAndHospitalCapacity"
* title = "Patient Impact and Hospital Capacity"
A measure is expected to be documented, and that documentation should contain the details necessary for implement the measure itself.
* relatedArtifact[0].type = http://hl7.org/fhir/ValueSet/library-type#documentation
* relatedArtifact[0].url = "https://web.archive.org/web/20200501215043/https://www.cdc.gov/nhsn/acute-care-hospital/covid19/"
* relatedArtifact[0].label = "NHSN COVID-19 Reporting" // Descriptive Text to display in a Link
* relatedArtifact[0].display = "CDC/NHSN COVID-19 Patient Impact & Hospital Capacity Module Home Page" // Title of the link target page
Multiple relatedArtifact elements can be provided, the text above shows only the first of four relatedArtifact entries included in the actual example measure.
Every measure must have at least one Library resource conforming to the PublicHealthMeasureLibrary profile that provides the essential value sets and other resources that may be used to evaluate the measure. Details about the measure library for this sample measure can be found in the Sample Measure Library page.
* library = "http://hl7.org/fhir/uv/saner/Library/ComputableNHSNMeasureLibrary"
This measure first addresses the Impact of COVID-19 on hospital patients, stratifying data by hospital location (inpatient vs. ED/Overflow), ventilation status, and patient death on the date of reporting.
There are multiple sets of patients to report upon for this section.
The initial patient population is Patients in the Hospital with Confirmed or Suspected COVID-19.
Patients on a ventilator are of interest, patients not on a ventilator are a stratum that need not be counted because that number can be determined mathematically from the data already provided.
Each of the values above is essentially counting an event, an admission to a location, or such admission with the use of ventilator equipment, or a death, but are not reporting cumulative totals. These would then be reported as different cohorts with potentially overlapping values.
Patients who acquired COVID-19 while in the hospital are a separate strata from patients on a ventilator.
The Venn Diagram below illustrates the different subsets of patients in this measure.
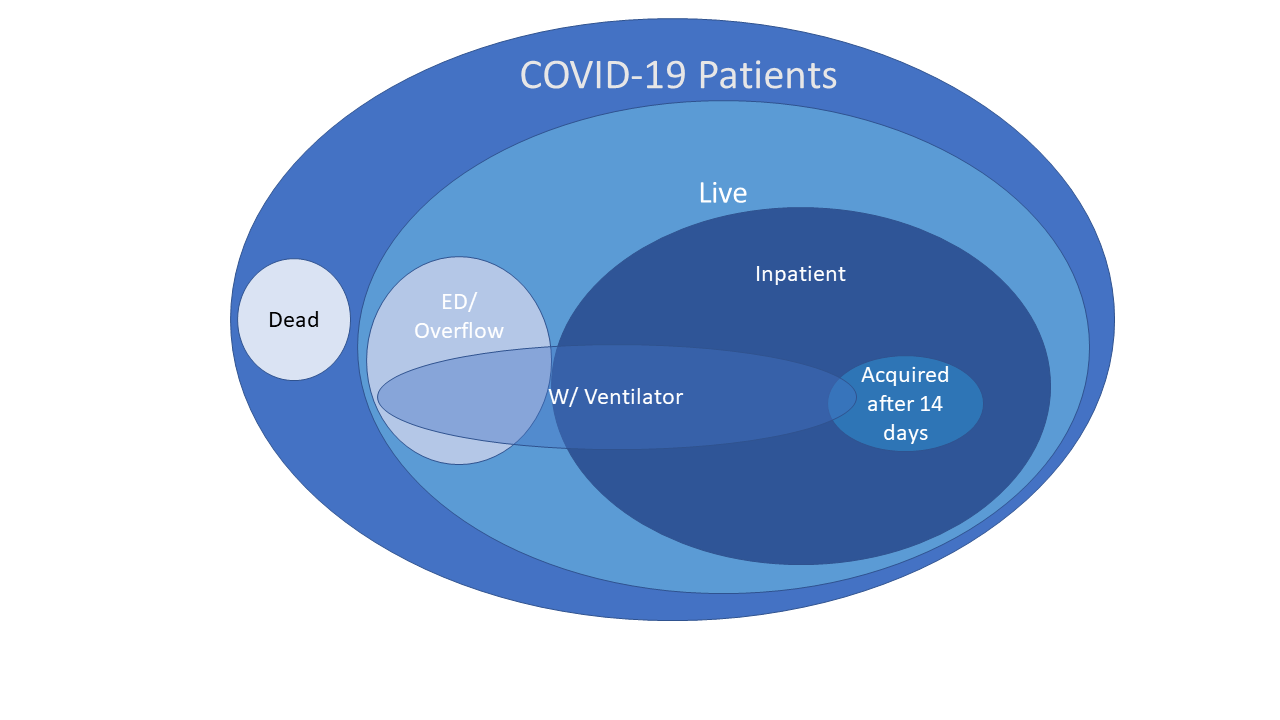
To simplify this section, this measure should be divided into at least three separate groups. Each group and stratum is preceded by the name used to identify it.
The next section of this measure addresses hospital capacity with respect to all beds, inpatient beds, ICU beds, and ventilators. These are all clearly Capacity and Utilization measures. It can be clearly divided into two groups, with stratification of the Bed group in across three categories to support all reporting needs.
This portion of the measure makes two assumptions: the total number of licensed and staffed beds and ventilators changes infrequently, and that measure data is reviewed and adjusted (e.g., to account for institutional changes in staffing levels or bed counts) before being sent forward, so that prior measure reports and transmission review processes can be used to manage counts of total beds or ventilators).
Beds: Utilization of Beds in the different locations.
NOTE: The requested data for Beds is at different levels than the proposed measure. However, the data request is accessible from the proposed location categories below as follows:
These are provided in a different order in the measure because the group for Beds builds on a similar framework as is used for Ventilators, but includes complexity around stratification.
NOTE: The Beds group uses strata to reduce repetition in this exposition. However, this would prevent further stratification by social determinants such as age, race, ethnicity and gender. Any stratification layer can be “bumped” up a level into a numerator population by the addition of a final filter by the criteria which distinguishes it.
.where(fieldToStratifyBy = 'ValueToMatch')