This page is part of the International Birth And Child Model Implementation Guide (v1.0.0-ballot: Releases Ballot 1) based on FHIR (HL7® FHIR® Standard) v5.0.0. No current official version has been published yet. For a full list of available versions, see the Directory of published versions
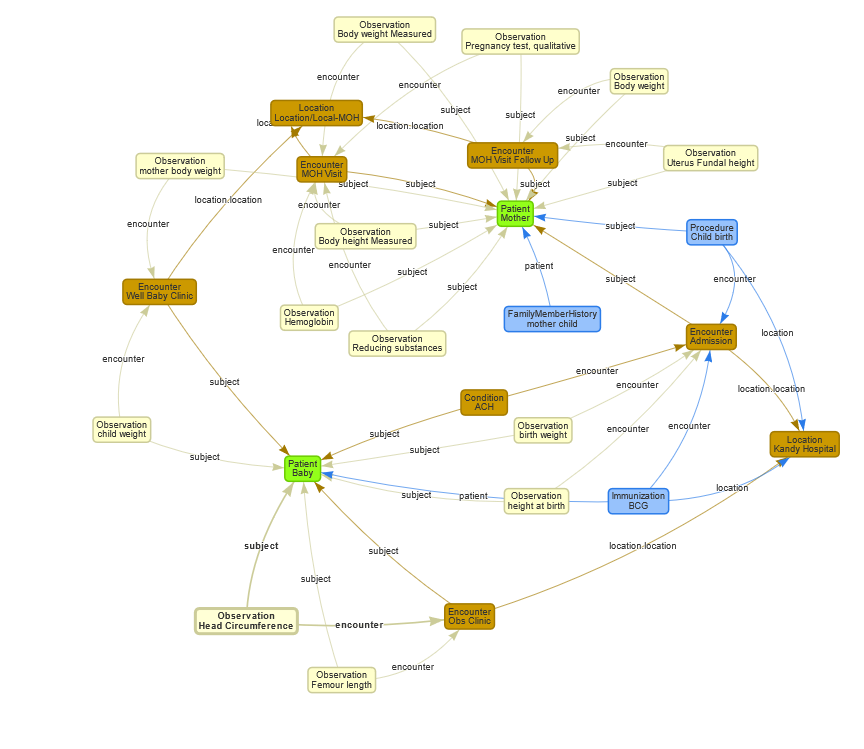
This use case is a basic use case where you communicate data from one system to another system. Usually such a data transfer is a combined set of data with information about the mother, the pregnancy or the fetus.
MS is a female known with Achondroplasia. She was born to a healthy couple and diagnosed in early childhood. She is married to a healthy male and currently lives in Kandy Sri Lanka. She G1P0 (first pregnancy). Her birthday is 1991-02-01. She is employed at a tea estate as a tea plucker. Her mobile number +94775588745 and address is 88, Factory Road, Peradeniya. Her husband is a healthy male.
MS Birth At birth MS was a floppy baby and had macrocephaly and short limbs. A Complete skeletal survey (83020-8) was done and revealed short femur and humerous, squared off iliac wings and short proximal and middle phalanges Achondroplasia was diagnosed based on the clinical and x-ray findings.
Achondroplasia management From birth until the age of 12 years she was managed at the paediatrics clinic of the Teaching hospital Kandy under a pediatrician. Beyond the age of 12 her management was handed over to the adult medical clinic of the same hospital. After reaching the age of 18 years her follow-up to the clinic was not done properly as she had to find a job.
Pregnancy diagnosis and Clinic engagement – 8 Weeks of POA MS got married at the age of 29 years. And got pregnant in the next year. Pregnancy was diagnosed by a urine HCG test. She was registered to the local Medical Officer of Health (MOH) office. Baseline examinations and testing done such as Weight, height, Hb, Urine for sugar.
First visit to Obstetrician at Teaching hospital Kandy. - 14 weeks of POA MS was registered at the Obstetric clinic in the Teaching Hospital Kandy. The basic investigations done. VDRL, HIV, Obstetric US Scan.
Continued monthly follow up at MOH office MS continued the pregnancy follow up at local MOH clinic. Other than general wellbeing, fetal growth by examination and maternal body weight is measured.
Second visit to Obstetrician at Teaching hospital Kandy. - 24 weeks of POA Anomaly US Scan was done. FL was slightly reduced. Planned to RV at 32 weeks.
Continued monthly follow up at MOH office MS continued the pregnancy follow up at local MOH clinic. Other than general wellbeing, fetal growth by examination and maternal body weight is measured.
Second visit to Obstetrician at Teaching hospital Kandy. - 32 weeks of POA
Third visit to Obstetrician at Teaching hospital Kandy for US Scan. Both FL and HC is increased. Planned EL/LCSC at 38 weeks.
Admission to Teaching Hospital Kandy for EL/LSCS – 38 weeks of POA MS was admitted to the hospital as requested for LSCS. She gave birth to a live boy. Uneventful LSCS The boy was floppy, had short limbs with proximal shortening and macrocephaly. (Standard data collected after birth in Sri Lanka)
MS MS Discharged – 1 day after EL/LSCS MS was discharged next day and asked to be followed up at medical clinic at Teaching hospital Kandy for achondroplasia follow up. Baby Discharged – 3 days after EL/LSCS
The paediatrician ordered complete skeletal survey to confirm the diagnosis is achondroplasia.