This page is part of the Clinical Guidelines (v1.0.0: STU 1) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.0.0. For a full list of available versions, see the Directory of published versions
Covered in this section:
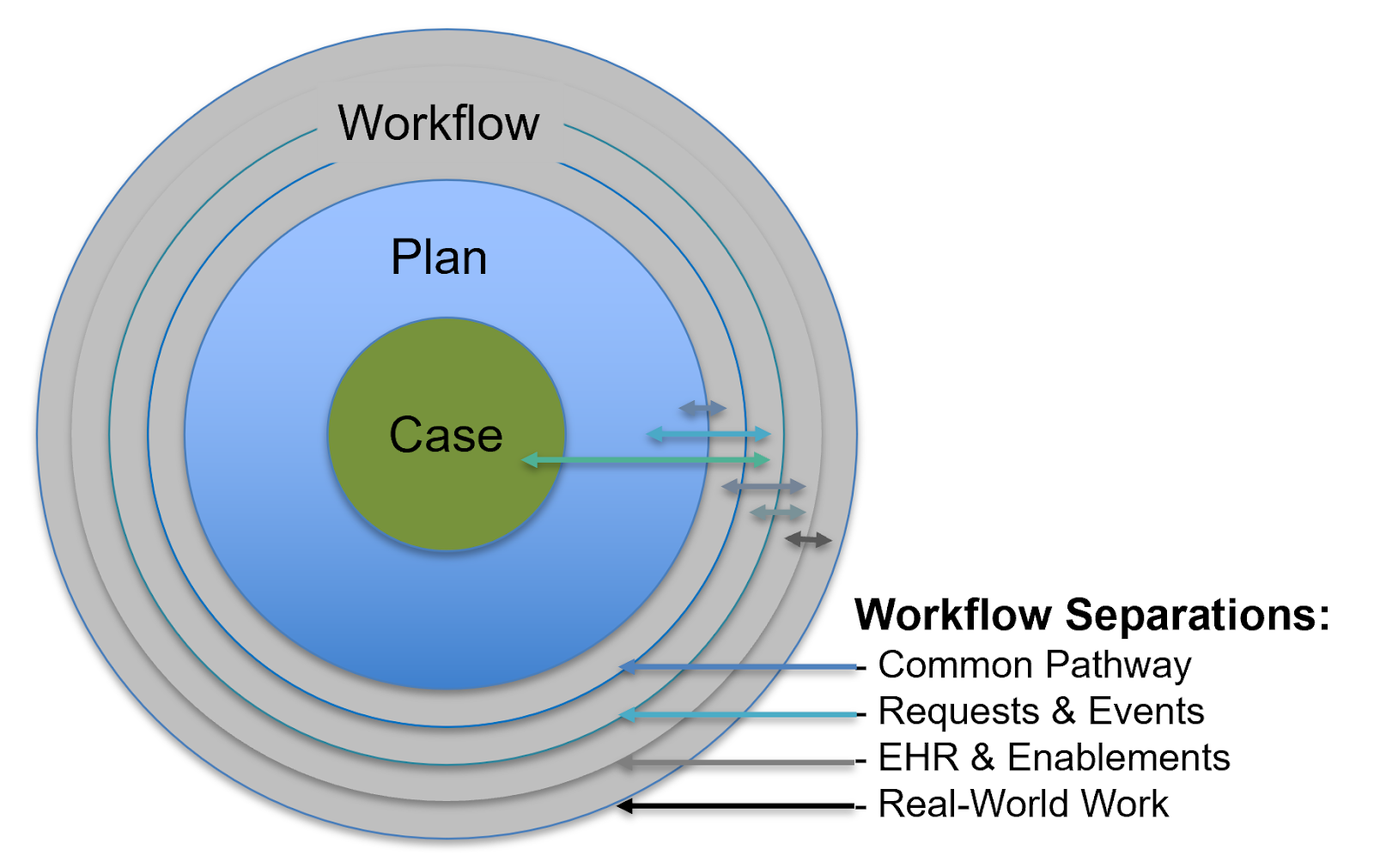
The workflow separation, as discussed in the section on Separations of Concerns in the CPG , is critical to address as a separation from the Case and the Plan as well as have means to relate to from the Plan and patient-specific Care Plan without conflating what is done for the patient with how it gets done (in local implementations). Workflow directly relates to the Case in that influences what is known about the patient (i.e., Events) and done for the patient (i.e., Requests) as well as when, by whom, where, and through what means. Thus, some aspects of local workflow can be inferred from information in the Case (e.g., CPGCaseFeatures).
Workflow itself may be further separated into generalized abstractions of workflow across settings and the real-world care delivery activities in those activities that are carried out in the context of clinical information systems (e.g., EHRs). The Common Pathway addresses higher level abstractions on care settings, clinical activities, and healthcare professional roles. Many implications of localized, real-world workflow are reflected in the information carried in FHIR Resources and related modules and patterns that are addressed in the FHIR Workflow Module including the FHIR Workflow Description, and its workflow resource patterns for Definitions, Requests, and Events. The Clinical Reasoning Module addresses the type of workflow interventions and/or enablements through which guidance is delivered into the care delivery process, such as the cardinal types of CDS1, described in part in its Common Use Cases.
Note that the Case and its associated data as defined by case feature groups and/or case features can be used to generate a case report at the end of the pathway. This approach SHOULD be aligned with the eCaseReporting implementation guide.
Such a case report could potentially include elements from the pathway view, such as things that have been ordered but not necessarily done, and recommendations that have not necessarily been followed. Although most of what a case report would be interested in would be case feature data, the ability to communicate items from the pathway view may have value in terms of understanding why recommendations are not being followed.
Note also that the case report could potentially include contextual elements such as local settings and configurations that were used when following guideline-based care.
The common pathway provides an abstract or generalized description of the overall process of care delivery that relates to care settings and high-level care activities. The common processes identified in this implementation guide are based on surveys of guideline content, both in the examples used in this guide, as well as other guideline content from various clinical domains and guideline authors.
The result is the definition of a Common Pathway that is intended to be applicable in any guideline-based care content, but not a specific localization or implementation thereof. Using this common pathway, content can indicate where in the overall process of care delivery a given recommendation or intervention should occur.
Content conforming to this implementation guide SHALL identify processes using the Common Processes code system.
Some local implementations of Pathways have used a similar approach using a work domain ontology to create a separation between the high-level descriptions of clinical workflow and the details of numerous, varying distinct interventions or enablements of specific workflows across clinical information systems, roles, and specific settings (e.g., units within the same hospital). A work domain ontology is a ‘shareable conceptualization’ of a setting where actual work occurs such that it can be discussed, described, analyzed, modelled, governed, and supported (e.g. with information and knowledge management tools) effectively- in part, through use of consistent, common, and sufficiently detailed vocabulary. Where available, publicly available standard vocabularies and ontologies were used to describe settings, roles, activities, and information system components (including user interface and data elements).
In these contexts, a work domain ontology was used as a means to normalize the various distinct findings from the numerous task or workflow elicitation and analysis methods and efforts (ref ), that can then be used to related to guideline-directed cognitive and decision support enablements (ref). Generalizations can be further specified or localized using site-specific logic including for specific triggering events and interventions. Further details of localization are site, vendor, and mechanism of integration specific and are currently beyond the scope of this implementation guide.
Tracking of workflow as performed in the clinical information system (i.e. EHR) is described in the FHIR Workflow Description. This topic is covered in depth in the FHIR Workflow Module. This implementation guide briefly describes its implications for the CPG.
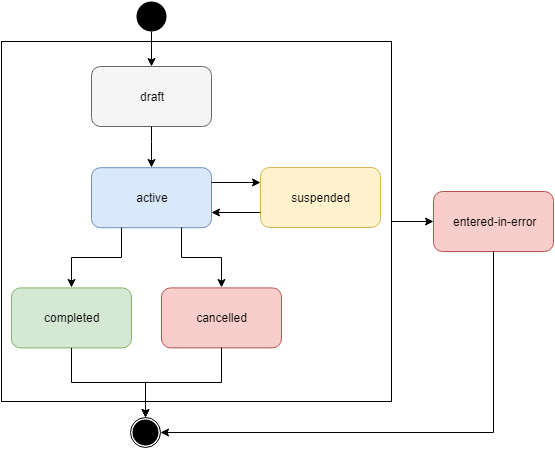
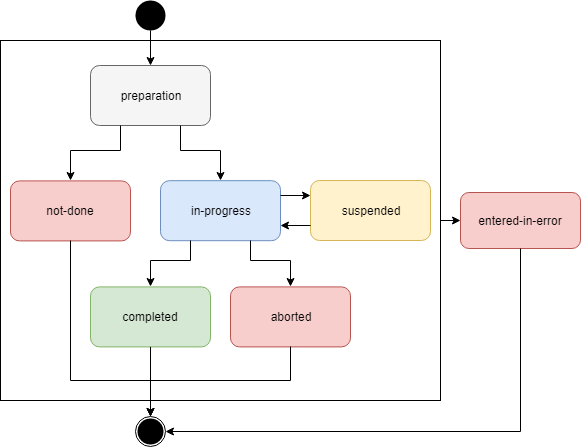
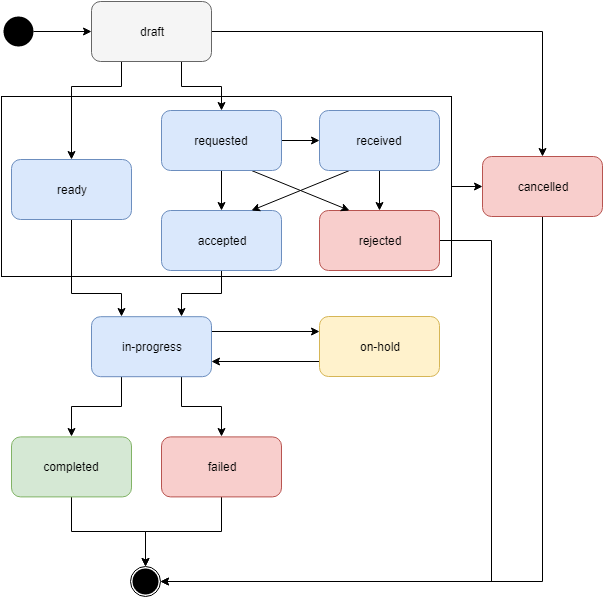
The things being done in the clinical information system are called activities and are defined using the FHIR ActivityDefinition resource. The ActivityDefinition provides the description or definition of an action to be performed and is applied to a FHIR resource following the Request and/or Event patterns. The workflow relationships of FHIR resource patterns involved in Activities including Definitions, Requests, and Events is described here. The FHIR Request pattern has a status that uses a defined value set. Request Status includes: draft, active, on-hold, revoked, completed, entered-in-error, and unknown that can be described as a state machine. The FHIR Event pattern likewise has its own status that uses a scoped value set that can be described as a specialized state machine. THe Event status includes: preparation, in-progress, not-done, suspended, aborted, completed, entered-in-error, and unknown. These patterns are described in the figures below.
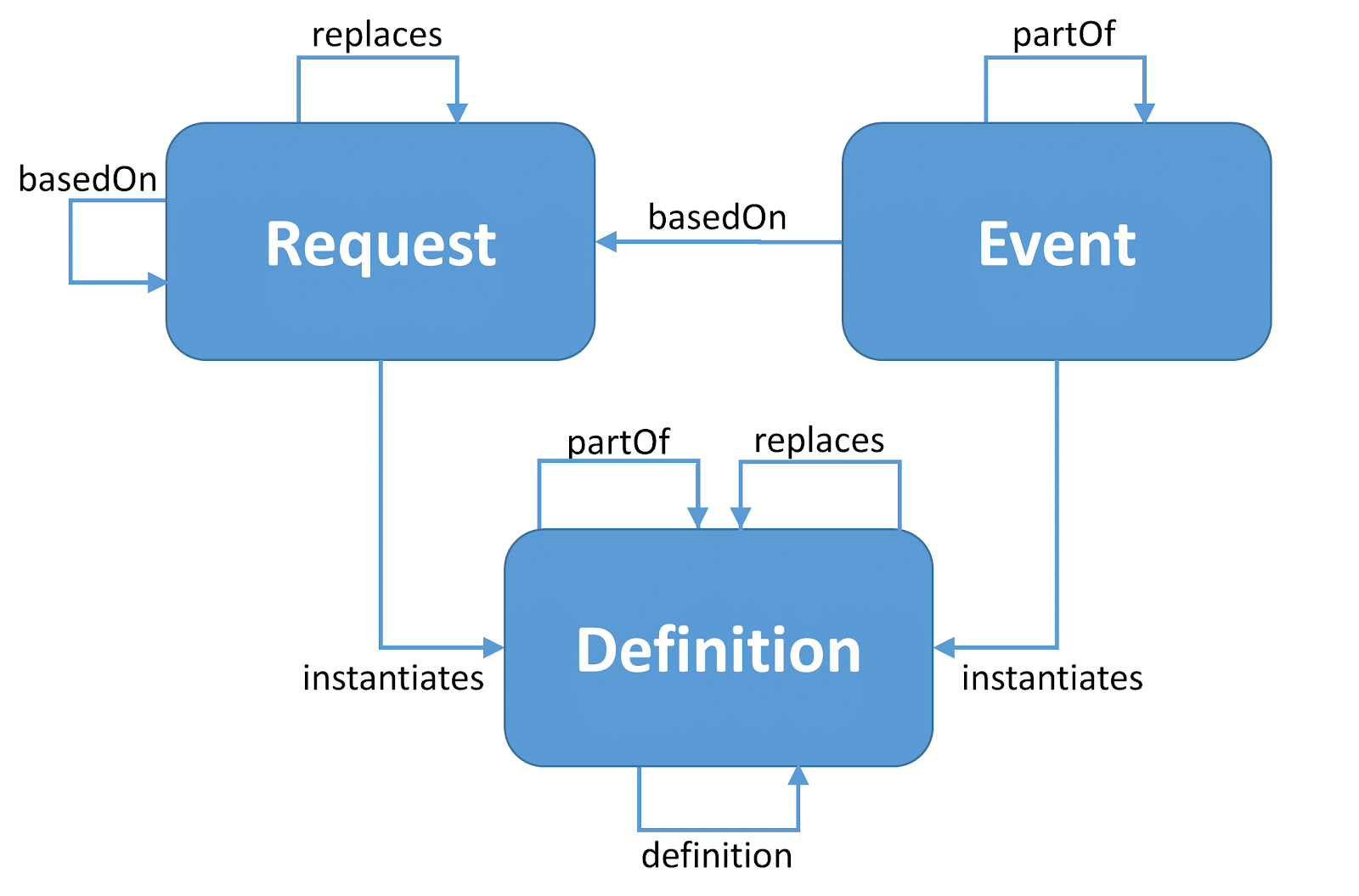
Further tracking of the state of completion of an activity may be supported through the FHIR Task Resource which may be applied to a Request as well as its resulting or related Events. A Task resource describes an activity that can be performed and tracks the state of completion of that activity. It is a representation that an activity should be or has been initiated, and eventually, represents the successful or unsuccessful completion of that activity.
Tasks are related to Requests in that tasks can both request and track the fulfillment of a request. In some cases, fulfillment may also result in the creation of sub-tasks. Requests do not track their own fulfillment - i.e. requested/accepted/in-progress. This is managed through Task. The status of a request only reflects the status of the “authorization/intention”, not how the request is being executed or not. It is possible for multiple tasks to be associated with the fulfillment of a single Request.
Tasks are related to Events in that events can be performed in fulfillment of a task and performing an event may involve the execution of one or more tasks. Events do not track the fulfillment of any requests they may be associated with. Tracking of fulfillment is managed through the Task resource.
The FHIR Task resource also has its own status that uses a scoped value set that can be described as a specialized state machine. Tasks can further carry information about Intent that uses a scoped value set including: plan, proposal, order, original-order, reflex-order, filler-order, instance-order, optional, and unknown. Task Status and Intent can be used to address boundary issues related to workflow in a CPG. Boundaries and relationships related to Taks and their use with Requests and Events are further discussed in the Task resource section on Boundaries and Relationships.
As described above, much information about clinical information system workflow may be carried in the FHIR Request and Event resources that interoperate between clinical information systems and/or decision-support services and apps (e.g., CDSHook, SMART-on-FHIR apps). And the Task resource describes activities that can be performed in these systems and can track the state of completion of these activities. The CPG recommendations and their associated requests and events are such activities that can be directed or enabled through various workflow interventions.
The Clinical Reasoning Module addresses the type of workflow interventions and/or enablements through which guidance is delivered into the care delivery process, such as the cardinal types of CDS (ref) (e.g., alerts and reminders, order sets, documentation templates, smart forms, information summaries- often problem or intervention oriented), quality or performance measurement or patient-level metrics or indicators, or more advanced forms of workflow or cognitive support delivered via apps adjacent or supplemental to clinical information systems (e.g., SMART-on-FHIR Apps). Further considerations for these interventions or enablement may include the “CDS five rights”: the right information; to the right person; in the right intervention format; through the right channel; and at the right time in the workflow2.
In the CPG implementation guide, these interventions and enablement are recognized to be downstream consumers of the knowledge content within the CPG with considerations being made for critical content or information requirements thereof. Many of these interventions or enablements have their own standard and/or implementation guides (CDS-Hooks, SMART-on-FHIR, Measure IG, eCaseReport-IG). While the CPG-IG intentionally does not directly address details of localized clinical workflow, it must and does provide affordances conveying critical content for downstream consumers including “the Common Pathway” (i.e., an abstraction of high-level clinical workflows), shared information (e.g., Requests and Events as CPGCaseFeatures), and reuse of the same standards for clinical information system activities (e.g., requests, events, and their lifecycle including their status and tasks) as well as interventions (e.g., forms, CDSHooks, etc.).
1: Osheroff, J. A. (2012). Improving outcomes with clinical decision support: an implementer’s guide. HIMSS
2: Campbell, R. J. (2013). The five rights of clinical decision support: CDS tools helpful for meeting meaningful use. Journal of AHIMA, 84(10), 42-47