This page is part of the Clinical Guidelines (v0.1.0: STU 1 Ballot 1) based on FHIR R4. The current version which supercedes this version is 1.0.0. For a full list of available versions, see the Directory of published versions 
This implementation is organized with the following sections, accessible via the menu bar at the top of every page:
This implementation guide supports the development of standards-based computable representations of the content of clinical care guidelines. Its content pertains to technical aspects of digital guidelines implementation and is intended to be usable across multiple use cases across clinical domains as well as in the International Realm.
This implementation guide has been developed through a multi-stakeholder effort, holistically involving a range of stakeholders, including those who work at the beginning of the process (e.g., guideline developers) to the end users (e.g., clinical implementation team representatives, health IT developers, patients/patient advocates), and others in between (e.g., informaticists, communicators, evaluators, public health organizations, clinical quality measure and clinical decision support developers).
The premise involves determining the representation of clinical practice guideline recommendations in FHIR as part of an iterative guideline development and implementation process (Figure 1.1). By including all the relevant perspectives (e.g., guideline authors, informaticists, implementers, communicators, evaluators) as part of the iterative process, the resulting computable representation of the recommendations should be well-vetted and more readily implemented.
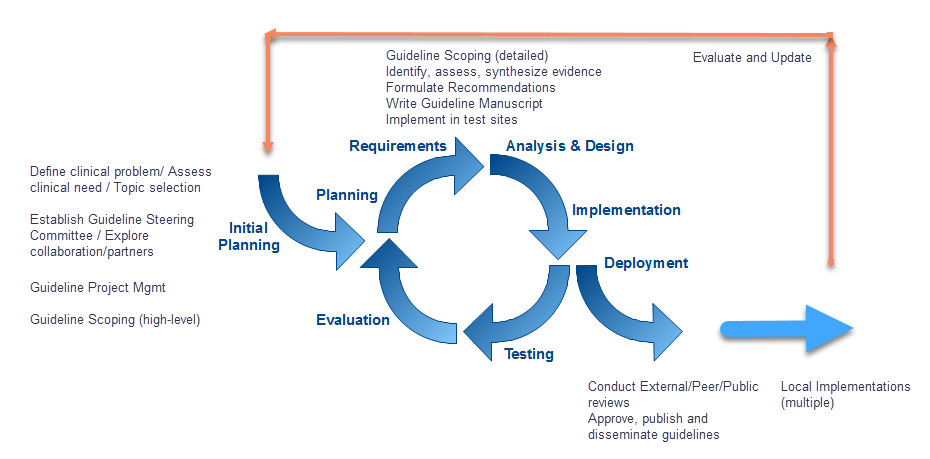
Figure 1.1
The implementation guide focuses on establishing patterns, profiles, conformance requirements, and guidance for the patient-independent representation, and analogous patterns for the patient-specific representation of guideline recommendations.
Direct:
Indirect:
Clinical informaticists, health system integrators and clinical systems developers. Assumes familiarity with relevant standards, including FHIR and Clinical Quality Language (CQL).
The need for computable care guidelines can be considered in the context of the data lifecycle, where the representation of the guideline recommendations in FHIR helps deliver actionable knowledge (Figure 1.2).
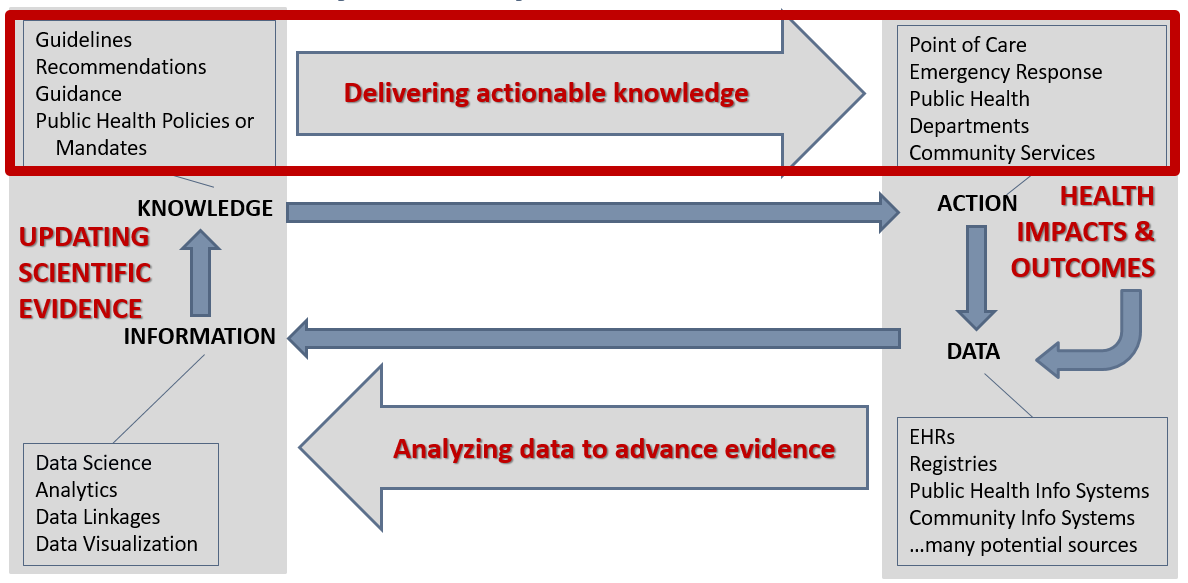
Figure 1.2
By translating the recommendations in clinical practice guidelines at the source, and disseminating a computable version along with the narrative version of the guidelines, the effort of translation would not be repeated across every organization that intends to apply the recommendations. Likewise, unnecessary or unintentional variations as a result of duplicative translation efforts could be prevented with a standard, computable version that is ready to be implemented. In removing the need for translating recommendations at each local clinical system, and removing as much variation as possible through a standard translation, the time needed to apply the recommendations in practice should also be reduced, helping scientific evidence reach patient care more easily, quickly, accurately, and consistently.
In considering common patterns across multiple guidelines, this implementation guide can apply to a variety of use cases across multiple clinical domains, as is evidenced by the examples provided. These common patterns not only create a way to organize the content for the translation into computable recommendations but also help implementers operationalize the recommendations within clinical workflows.
| Author Name | Affiliation | Role |
|---|---|---|
| J. Rex Astles, PhD, FAACC | CDC, Health Scientist | Contributor |
| Wendy Blumenthal, MPH | CDC, Health Scientist | Contributor |
| Matthew M. Burton, MD | Apervita, Inc., VP Clinical Informatics | Contributor |
| Zahid Butt MD, FACG | Medisolv Inc, CEO | Contributor |
| Dave Carlson, PhD | Clinical Cloud Solutions, Solution Architect | Contributor |
| Daryl Chertcoff | HLN Consulting, Solution Architect | Contributor |
| Jeffrey Danford, MS | Allscripts, Sr Principal Software Engineer | Contributor |
| Floyd Eisenberg, MD, MPH | iParsimony | Contributor, Co-Chair (Clinical Quality Information) |
| Margaret S. Filios, MSc, BSN, RN, CAPT USPHS | CDC, Senior Scientist | Contributor |
| Daniel Futerman | Jembi Health Systems, Senior Program Manager | Contributor |
| Joel C. Harder, MBA | AiCPG, Executive Director | Contributor |
| Aaron M. Harris, MD, MPH, FACP | CDC, Subject Matter Expert | Contributor |
| Dwayne Hoelscher, DNP, RN-BC, CPHIMS | Nursing Informaticist | Contributor |
| Emma Jones RN-BC, MSN | Allscripts, Expert Business Analyst | Contributor, Co-Chair (Patient Care), IHE Co-Chair (Patient Care Coordination) |
| James Kariuki | CDC, Health Scientist | Contributor |
| Kensaku Kawamoto, MD, PhD, MHS | Contributor, Co-Chair (Clinical Decision Support) | |
| Robert Lario, MSE, MBA | University of Utah/US Department of Veterans Affairs, Health Standards Architect | Contributor |
| Ira M. Lubin, PhD | CDC, Health Scientist | Contributor |
| Laura Haak Marcial | RTI International, Health Informaticist | Contributor |
| Robert McClure, MD, MPH | Contributor, Co-Chair (Vocabulary) | |
| Maria Michaels | CDC | Contributor |
| Blackford Middleton, MD, MPH, MSc, FACP, FACMI, FHIMSS, FIAHSI | Apervita, Chief Informatics & Innovation Officer | Contributor |
| Nikhil Patel MBBS, BSc | NHS, Physician | Contributor |
| Bryn Rhodes | Dynamic Content Group | Editor, Co-Chair (Clinical Decision Support) |
| Derek Ritz | ecGroup Inc., Principal Consultant | Contributor, IHE Co-Chair (Quality Reporting and Public Health) |
| Julie Scherer, PhD | Motive Medical Intelligence, Chief Informatics Officer | Contributor |
| Julia Skapik | Cognitive Medical Systems, CHIO | Contributor |
| Larie Smoyer, MD | Motive Medical Intelligence, VP of Product Development | Contributor |
| Jodi Wachs MD, FAAPM&R FAMIA | Clinical Informaticist | Contributor |