This page is part of the SDOH Clinical Care for Multiple Domains (v2.0.0: STU 2) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.3.0. For a full list of available versions, see the Directory of published versions
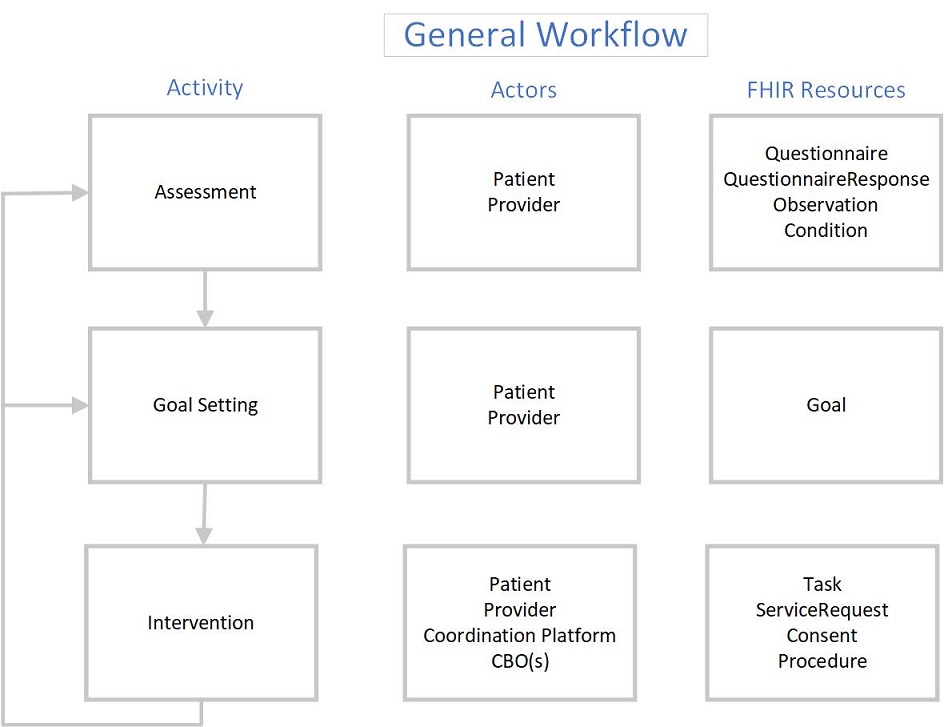
The following depicts the general workflow anticipated by this Implementation guide. The general process is to:
1) Assess the patient to determine social risk – this may be done by using an assessment tool or via a conversation with the patient, or both. As part of the assessment, the patient and provider agree on the specific risk items that are to be labeled as verified health concerns or problems.
2) The patient and provider may establish specific goals regarding the identified social risk.
3) The patient and provider agree on specific referrals/interventions that should be undertaken to address the problems and goals. The patient’s consent is obtained to share their specific information with the entity that will be performing the services. The provider then sends a task to the performing entity to initiate the electronic referral.
 |
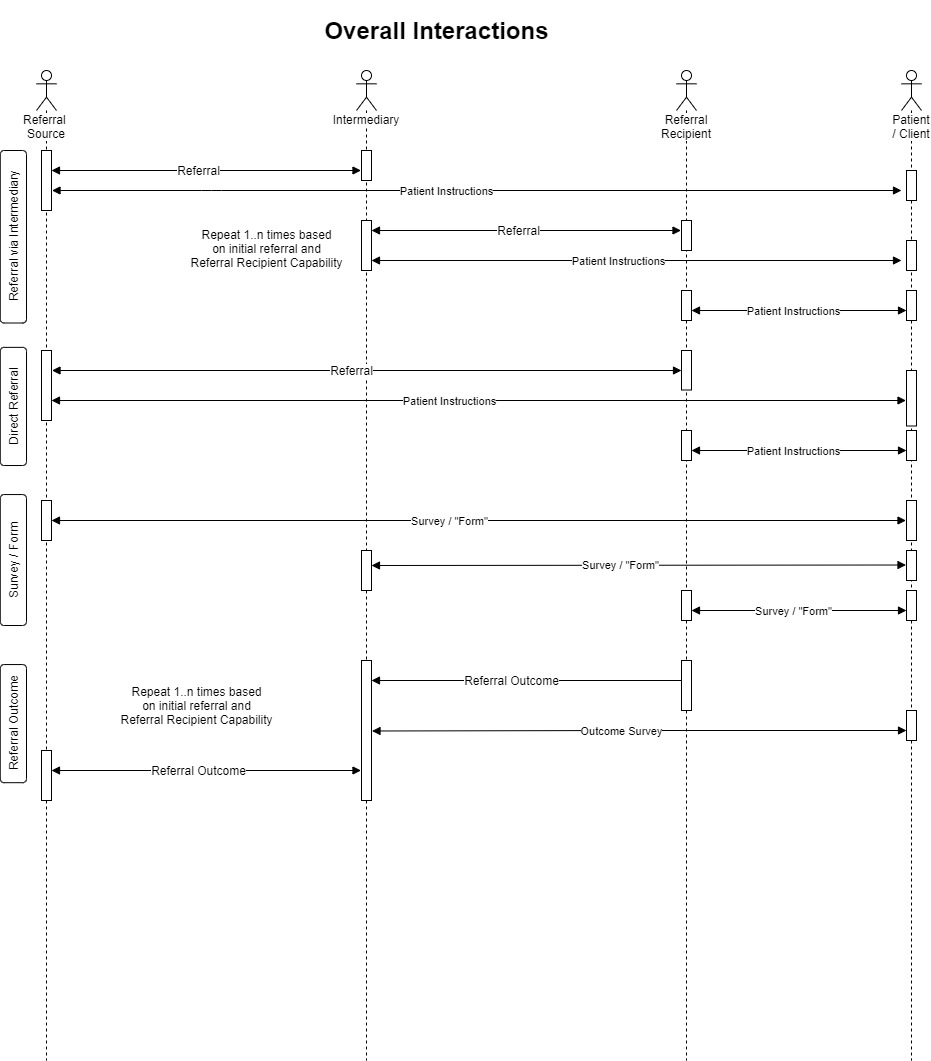
There are a number of system to system interactions supported by this implementation guide. These include:
 |
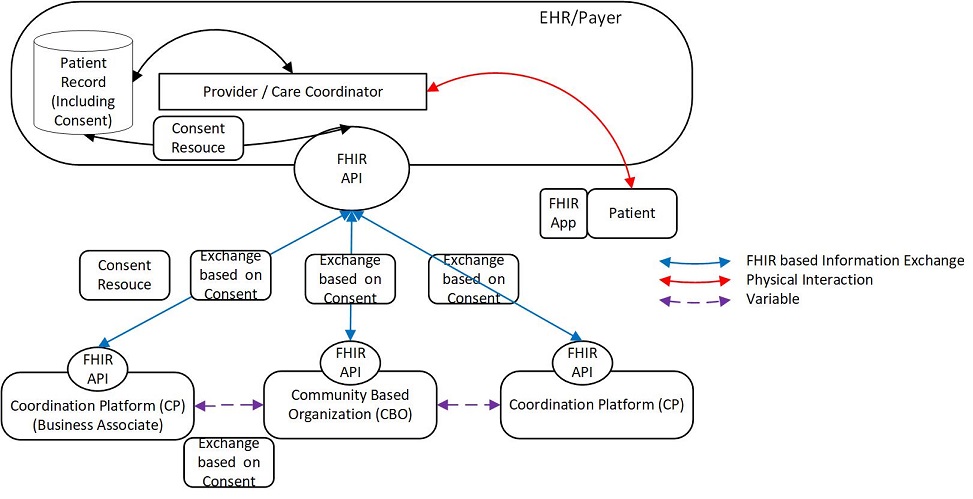
The Gravity Project recognizes the need to appropriately manage privacy and consent related to a patient’s social risk issues. This IG assumes that each organization has appropriate mechanisms in place to secure SDOH information and will only release it with appropriate consent. The Office of the National Coordinator (ONC) and HL7 International (HL7), and the Office of Civil Rights (OCR) (this is not an exhaustive list) have active programs in place to determine what needs to be done to protect all personal information (including SDOH) from inappropriate disclosure and use. In this version of the IG, we are providing a specification for a FHIR Consent resource that should be exchanged between a Covered Entity and a Business Associate (BA) when the patient has authorized the BA to release their information to a non-HIPAA covered entity. While this is not a complete treatment of the issues related to consent, it is a starting point to test the viability of exchanging consent information. Future versions of this IG will incorporate additional technical standards to support the protection and authorized release of SDOH information as they are developed by the ONC, HL7, and OCR. The diagram below illustrates the approach taken by this IG to exchange a Consent resource between a Covered Entity and its BA.
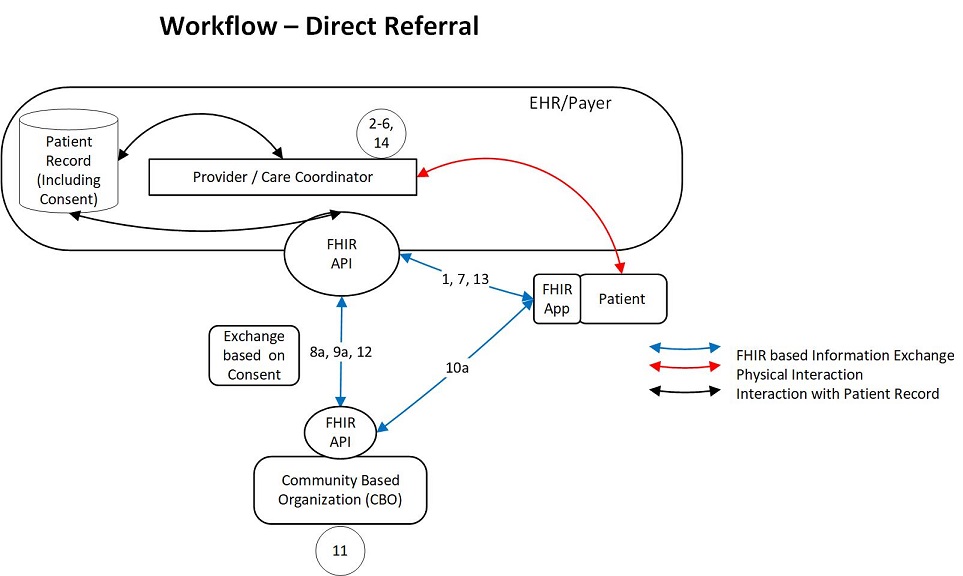
The following diagram depicts one example of an exchange workflow supported by this version of the IG.
 |
Each of the workflow diagrams below defines the resources that are exchanged and/or updated for the supported use cases.
Provider / Requester – this can be any of the following:
1) a provider or other provider
2) a payer as part of care management, risk assessment, or via programs that assess and intervene regarding social risk
3) a Coordination Platform
Coordination Platform (CP) / Intermediary
1) This is a service that accepts referrals (it may also create them)
2) May determine which Community Based Organization (CBO) is capable and available to provide the appropriate service
3) Engages the CBO to perform the referral
4) Tracks the referral process to completion
5) Reports status back to the Referring Entity
Community Based Organization (CBO) / Performer
1) Provides one or more social risk services
2) Interacts with the CP or RE to provide status of the referral
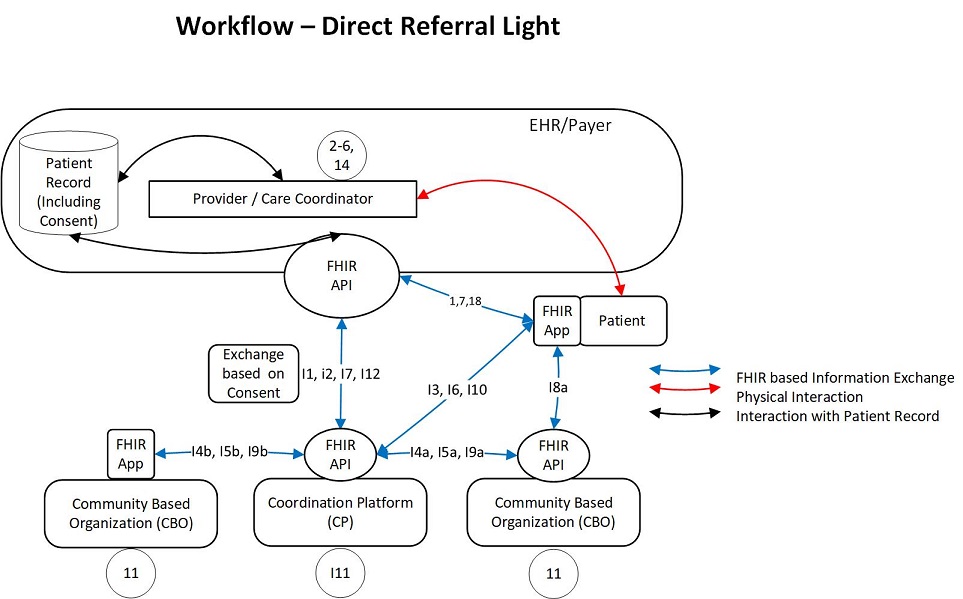
The referral occurs between the Provider / Requester and the CBO / Performer where the CBO has a FHIR API.
Link the Direct Referral functional use case
 |
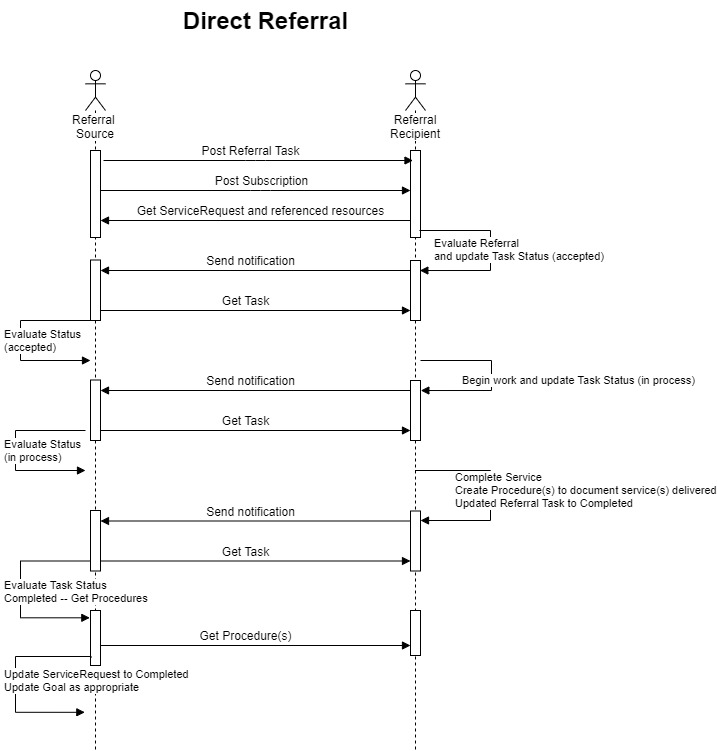 |
The referral occurs between the Provider / Requester and the CBO / Performer where the CBO / Performer does not have a FHIR API (FHIR Server or FHIR Façade). The exchange with the Performer is initiated via an email with a secure link to the Provider / Requester API that can be used by an application available to the CBO / Performer to communicate with the Provider / Requester using RESTful exchanges that read, create, and update resources via the Provider / Requester API.
Link to the Direct Referral Light functional use case
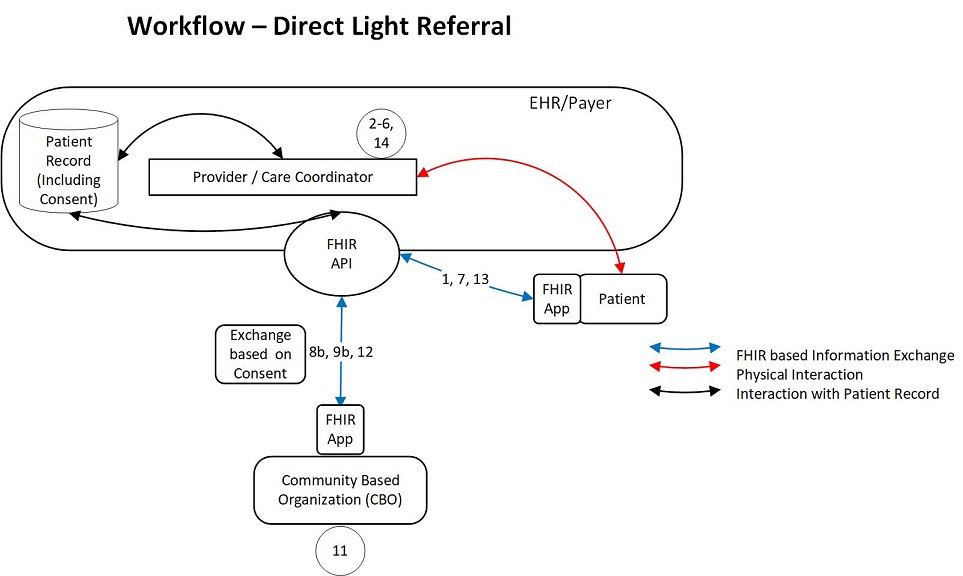 |
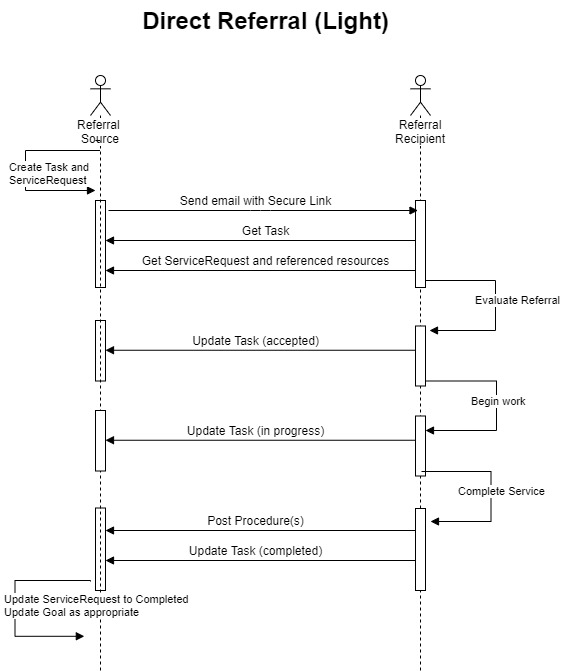 |
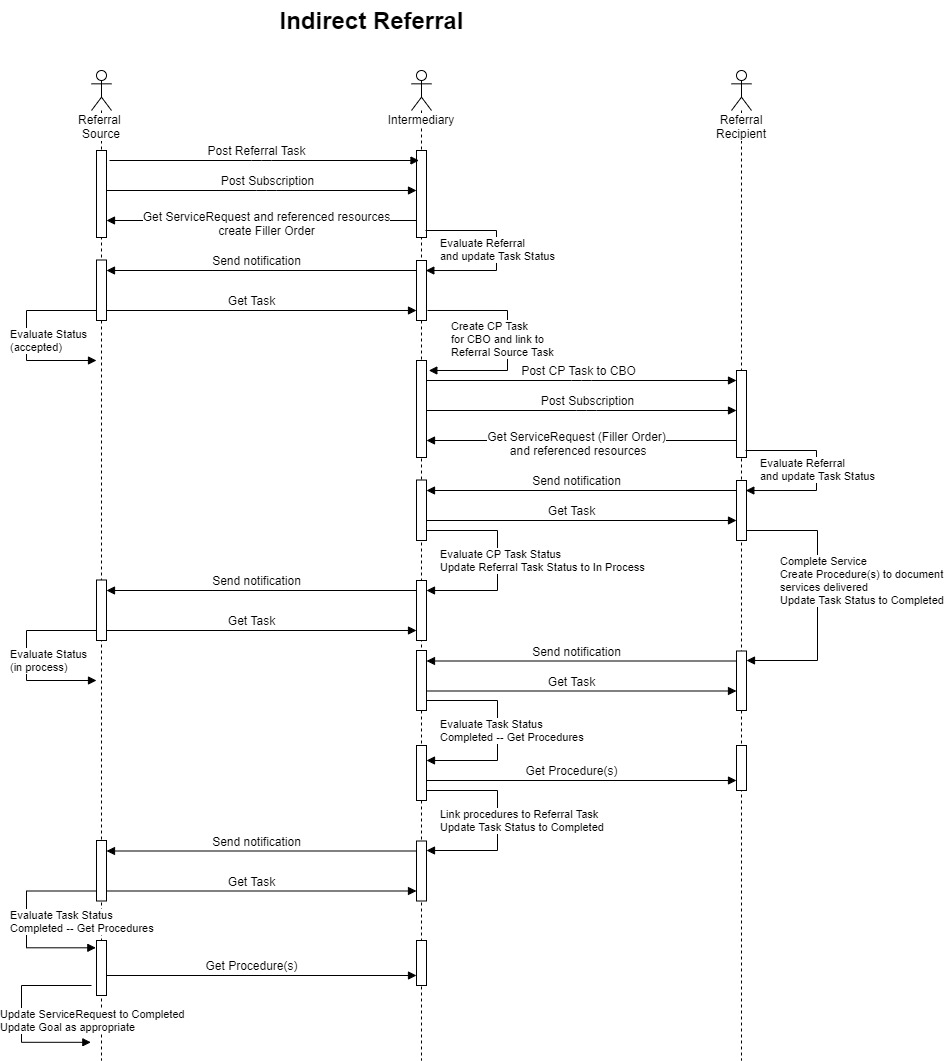
The referral occurs in two separate interactions. The first is between the Referral Source and the Intermediary and the second is between the Intermediary and the Referral Performer.
This IG assumes that, in an Indirect Referral, the Referral Performer does not have the ability to communicate directly with the Referral Source. Therefore, the intermediary SHALL support the following.
Link to the Indirect Referral with a Direct CBO functional use case
Link to the Indirect Referral with a Direct Light CBO functional use case
 |
 |
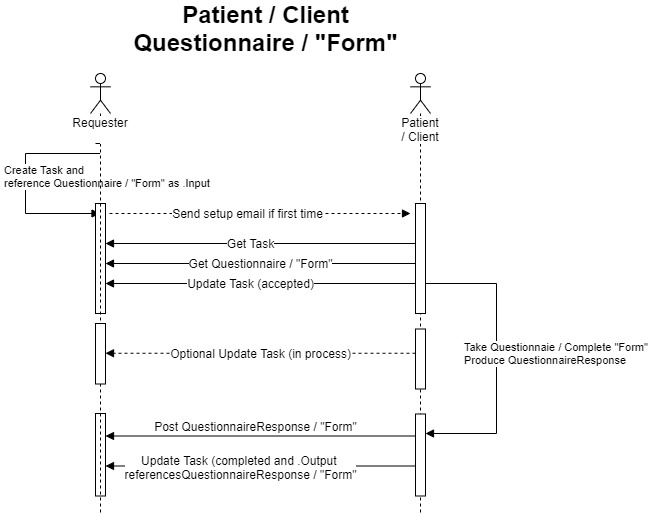
This implementation guide supports additional interactions with a patient/client application (on a smartphone or portal). These interactions include providing the patient/client with:
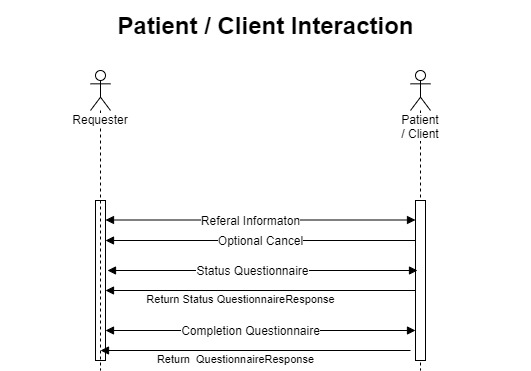 |
The above patient / client interaction diagram indicates the high level exchanges between the Requester and the Patient / Client:
 |
The Provider / Requester, CP / Intermediary, and CBO / Performer SHOULD make SDOH information available to authenticated and authorized APIs and applications via a FHIR API conformant to the ONC 21st Century Cures Act Final Rule. The API SHOULD allow for the exchange of all resources defined on the FHIR Artifacts Overview page with the patient’s consent where required or appropriate