This page is part of the PACIO Personal Functioning and Engagement Implementation Guide (v2.0.0: STU 2) based on FHIR (HL7® FHIR® Standard) R4. This is the current published version. For a full list of available versions, see the Directory of published versions
| Page standards status: Informative |
The Personal Functioning and Engagement IG defines the data structures for exchanging information related to an individual's functioning, both with respect to their body as well as their activities and participation in society. This includes observation data (characteristics that can be tested, measured, or observed and are communicated with a name-value pair structure) as well as related clinical care.
The following scenario illustrates one situation in which this IG enables sharing of important information across many care settings, focusing on long-term post-acute care (LTPAC) and health domains of interest in that setting, such as mobility, self care, mental functions, and communication.
Post-actute care (PAC) providers and caregivers in particular are interested in the functioning and engagement of their patients. PAC supports the recovery and rehabilitation of individuals and aims to enable them to live and act as independently as possible. To identify necessary interventions and track progress, PAC providers, caregivers, and payers collect and document observational data on the patient's abilities and interactions. However, as the following scenario illustrates, they interact with many other healthcare settings, which provide valuable information on a patient's functioning that informs ongoing care. Figure 1 illustrates a common scenario for an elderly patient, Betsy Smith, moving through the healthcare ecosystem.
The journey starts with Betsy in her home. She has a medical event that results in an emergency medical service (EMS) transport to Hospital A. After she is stabilized, Betsy's doctor recommends that she be discharged to her home with support for continued rehabilitation from PAC home health services. The home health agency (HHA) helps Betsy return to her home and coordinates care with multiple professionals and provider organizations, including her primary care physician, pharmacy, behavioral health provider, and outpatient dialysis provider. Home health nurses periodically complete formal Outcome and Assessment Information Set (OASIS) assessments per Centers for Medicare & Medicaid Services (CMS) requirements, tracking Betsy's functioning as she recovers, including her mental functions, self care, and communication abilities.
Betsy has another medical event at home and is transferred to Hospital B. Based on evaluations performed at the hospital, Betsy's doctors determine that she will need significant help to recover enough independence to return home. They recommend she transfer to a PAC skilled nursing facility (SNF). While admitted, the SNF completes Minimum Data Set (MDS) assessment instruments documenting Betsy's abilities and progress. Once sufficiently recovered, the SNF discharges Betsy and she returns home with the help of a variety of home and community-based services (HCBS). While receiving HCBS, Betsy's caregivers complete Functional Assessment Standardized Items (FASI) assessments.
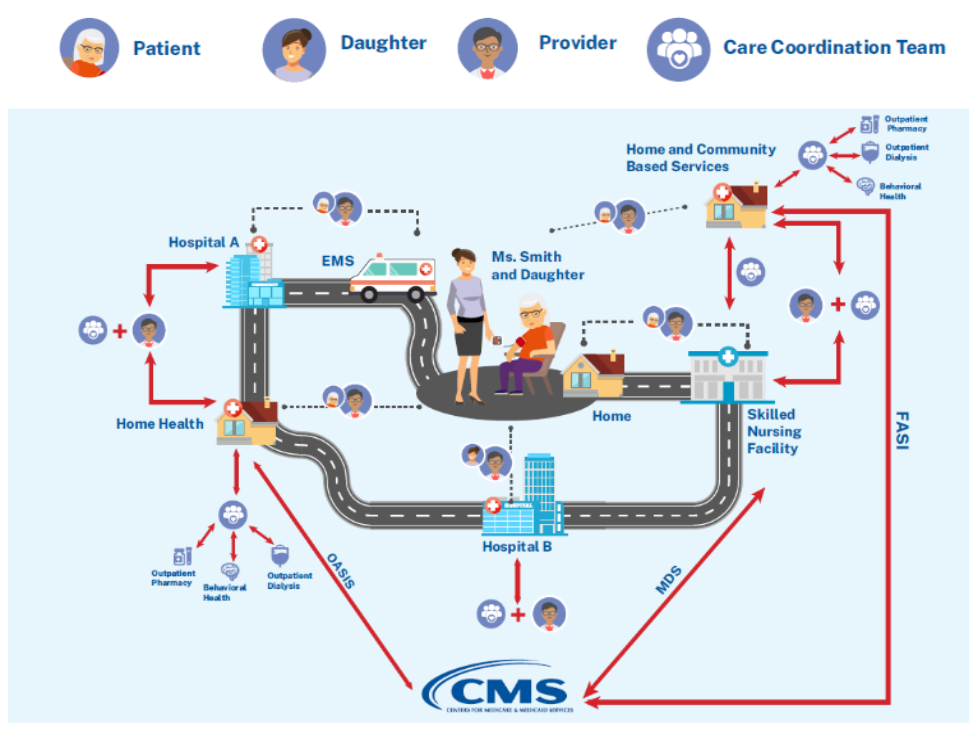
Figure 1: Example Post-acute Care Patient Healthcare Journey
Payers, such as CMS, require providers to perform and submit formal assessments, such as the MDS within SNFs, in support of claims for provided services. Using the collection and single observation profiles, the electronic medical record (EMR) systems in which clinicians capture these formal assessments can electronically transmit the assessments to, or make them available for access by, payers. The same approach can be used to electronically communicate MDS assessments by SNFs, FASI assessments by HCBSs, OASIS assessments by HHAs, or other formal assessments. Note that this capability does not constitute a requirement to exchange assessments electronically with CMS or other payers.
When patients transition between facilities and care organizations, it is important for data collected about their functioning to follow them in order to facilitate appropriate care by the receiving provider. Using the collection and single observation profiles, the EMRs in which clinicians capture these formal assessments can electronically transmit the assessments to, or make them available for access by, the receiving facility and its clinicians. The same approach can be used to electronically transmit MDS assessments by SNFs, FASI assessments by HCBSs, OASIS assessments by HHAs, or other formal assessments.
Because transitions usually occur between facilities of different types (e.g., SNF to HCBS), the receiving provider may not perform the specific assessments sent by the transferring facility. The categorization of observations into health domains defined by ICF enables recipients to organize data for display based on the categorization even if the specific observation code is not known by their system.
Family members and caregivers outside of formal healthcare settings provide essential care and support for individuals regaining their functioning and independence. Making data available using the collection and single observation profiles will allow FHIR-enabled applications to enable patients and their families to access information on their functioning. The categorization of observations into health domains defined by ICF enables these systems to present the information to users without understanding and administering complex assessment tools.