This page is part of the PACIO Advance Directive Information Implementation Guide (v2.0.0-ballot: STU 2 Ballot) based on FHIR (HL7® FHIR® Standard) R4. This version is a pre-release. The current official version is 1.0.0. For a full list of available versions, see the Directory of published versions
| Page standards status: Informative |
Mental health advance directives are legal documents that allow individuals to specify their preferences for mental health treatment in advance, in case they later become unable to make these decisions themselves due to mental illness. These directives can outline what types of treatments a person does or does not want, including medications, hospitalization, and therapies. They can also appoint a specific person, known as a healthcare proxy or agent, to make decisions on their behalf.
The main purposes of a mental health advance directive are to ensure that an individual’s treatment preferences are respected and followed during periods when they might not be able to communicate their wishes due to their mental health condition. This can provide reassurance to both the individual and their family, and can also help in preventing conflicts or confusion about the best course of action during a crisis.
The specifics of how to create and implement a mental health advance directive can vary by jurisdiction, so it is important to consult local laws and possibly seek legal advice when considering creating one or another.
The MHAD document structure is in an early stage with a primary focus on specifying the MHAD metadata with an unstructured advanced directive attached. We welcome feedback informing the structured representation of mental health sections.
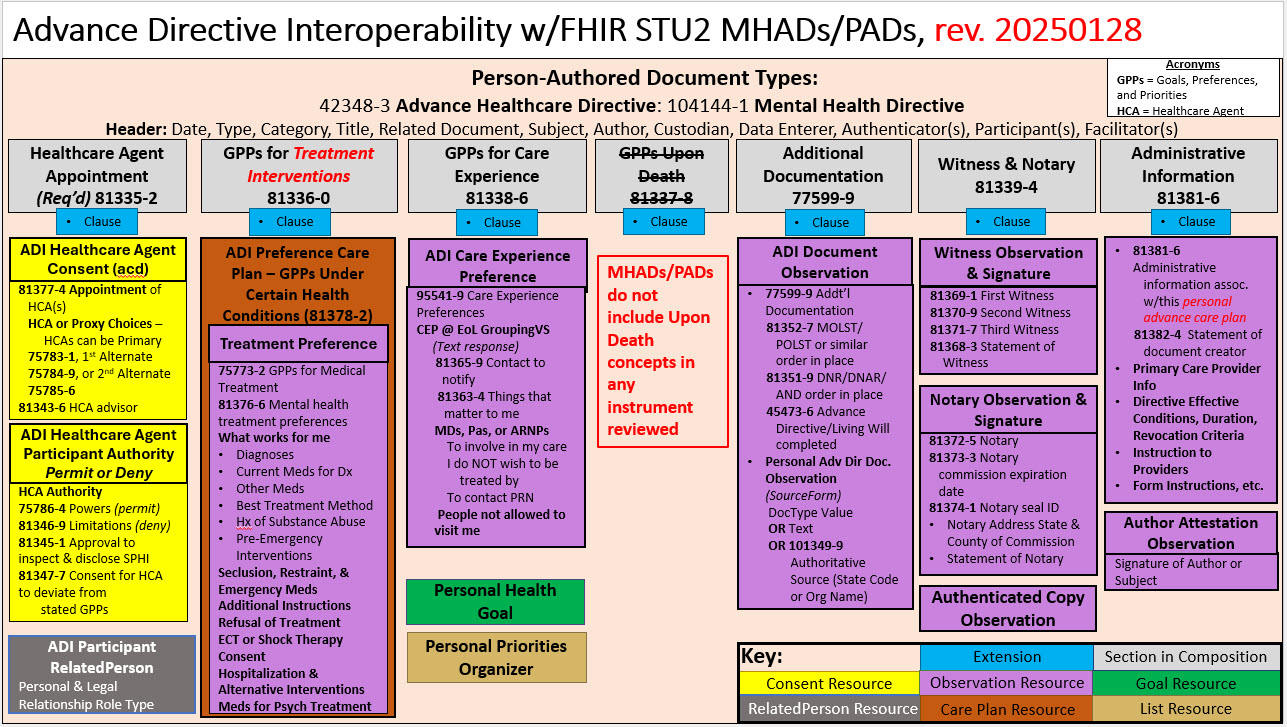
Structurally, MHAD shares the same ADI header as the PACP document. It differs in the related clauses. A summary of the document structure is shown below:
Personal Advance Care Plans - Systems used to create and update patient-generated advance care plans (PACPs) through a patient-directed process need a way for individuals to communicate information about their advance medical care goals, preferences, and priorities.
Individuals need a way to generate and update information related to their advance healthcare directives so that their current wishes can inform provider-generated care plans. Interoperable exchange of the advance directive documentation supports more effective sharing of this information across transitions of care and enables practitioners to create person-centered care plans that align with a patient’s values, goals of care, treatment preferences, and quality of life priorities when a patient can no longer communicate for themselves. Advance Directives – Person-authored advance directives (ADs) are legal or informal documents written by individuals, typically while they are still mentally competent, to outline their preferences for medical treatment in the event that they become incapacitated or unable to communicate their wishes.
These directives are a crucial component of advance care planning and aim to preserve patient autonomy at the end of life or during serious illness. A typical patient-authored AD may include:
Living Will: Specifies desired or undesired treatments (e.g., resuscitation, mechanical ventilation, tube feeding).
Durable Power of Attorney for Health Care (Health Care Proxy): Designates a trusted person to make decisions on the patient’s behalf.
Treatment Intervention Preferences: These represent the person's treatment intervention preferences to receive or not receive CPR when such a decision needs to be made, and often also contain other time-critical treatment orders related to life-sustaining treatment meant to restore, prolong, or sustain the life of the patient.
Personal Values Statements: Descriptions of what matters most to the patient, such as quality of life or religious beliefs.