This page is part of the Medicolegal Death Investigation (MDI) (v2.0.0-ballot: STU 2 Ballot) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.0.0. For a full list of available versions, see the Directory of published versions
In the investigation and certification of deaths, medical examiners, coroners, and other MDI professionals are in a unique position to provide specific and up-to-date mortality information to public health and public safety partners. However, despite the importance of this information to health and safety, the method of exchanging information between MDI organizations and stakeholders is disparate and includes paper-based and fax-based information exchange. Both public health and public safety communities are working to improve dataflows in a coordinated, consistent, and secure way across jurisdictional boundaries. The Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS) funded a series of pilot projects to explore the challenges and to test methods for medical examiner and coroner offices to send information to public health systems such as electronic death registration systems (EDRS) and for partners such as forensic toxicology laboratories to send information to medical examiner and coroner offices. The work involved identifying common data elements, creating data standards for those elements, and promoting interoperability between data systems.
In 2015, changes to the Office of the National Coordinator for Health Information Technology (ONC) criteria in the health information technology (IT) certification process led electronic health record (EHR) system vendors to implement FHIR standards and incorporate FHIR application programming interfaces (APIs) into their products for hospitals and other healthcare providers. In 2019, NCHS developed and implemented the FHIR standard for death reporting. The Vital Records Death Reporting (VRDR) FHIR IG was published in October 2020. That guide focused on the dataflow between vital record jurisdictions EDRS and NCHS.
Recognizing that many deaths of significant public health importance are investigated by medical examiner and coroner offices, NCHS is supporting the development of additional standards and to tools for interoperability within the MDI community and its data exchange partners. The CDC continues to support interoperability and data exchange modernization among medical examiner and coroner offices through the Collaborating Office of Medical Examiners and Coroners (COMEC). MDI community members interested in this work are encouraged to contact the COMEC at: MDI@cdc.gov.
This MDI FHIR specification is part of that effort to define elements and dataflows to standardize disparate systems within the MDI community.
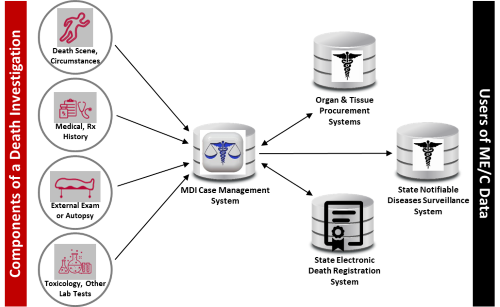
Medical examiner and coroner offices access and exchange information with multiple agencies and organizations when building a death investigation case record (e.g., law enforcement, forensic laboratories, EHR systems, jurisdictional EDRS). Case records are created in the MDI CMS and may contain entries from both internal sources (e.g., scene investigation) and external sources (e.g., laboratory analysis results).
Figure: Dataflows in the Death Investigation and Reporting System
 |
According to the U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics report, Medical Examiner and Coroner Offices, 2018, in 2018 2,040 medical examiner and coroner offices accepted 605,000 referrals for investigation to determine the cause and manner of death across federal, state, and local jurisdictions. The information gathered during a death investigation is useful to a variety of local, state, and federal agencies, and many entities rely on MDI-generated data. For example, the CDC monitors trends in unintentional injury, homicides, suicides, and sudden or unexpected infant deaths and develops policy recommendations and prevention strategies for such deaths. The National Highway Traffic Safety Administration (NHTSA) monitors trends in traffic-related fatalities and the U.S. Consumer Product Safety Commission (CPSC) uses mortality data to identify problematic products for investigation and potential recall.
MDI CMS vary by organization and location or jurisdiction, and these systems are often not interoperable with other producers or consumers of MDI-related data, which creates obstacles to timely investigations and forensic science research.
The scope of the current MDI IG is defining FHIR resources and guidance for the following dataflows:
The current project has place-holders for sections that are expected to have more detail in later versions, such as exam-autopsy results and narratives for death scene description and other uses. (See Further Work, below.)
The MDI specification supports exchange of data among organizations and agencies that contribute information to death investigations conducted by medical examiner and coroner offices as well as transmission of death investigation findings between MDI CMS and EDRS of state registrars. The Vital Records Death Reporting (VRDR) FHIR IG supports reporting deaths by state registrars to the NCHS. Therefore, the dataflows supported by the MDI specification are upstream of the dataflows supported by the VRDR specification. While the two IGs serve an overlapping set of actors (e.g., EDRS) and data concepts (e.g., death date, manner of death), they do not share profiles because VRDR data elements are constrained to IJE (Inter-Jurisdictional Exchange) data elements definitions.
Georgia Tech Research Institute (GTRI) provides tools for exploring and testing MDI FHIR data.
The MDI FHIR IG will continue to develop to support additional MDI needs beyond death reporting to EDRS for the death certificate. Future work likely will include:
This guide was developed and produced through the efforts of Health Level Seven (HL7) and created using the Trifolia-on-FHIR tool, provided by Lantana Consulting Group, Inc. The HL7 Project Insight reference number for this project is 1737.
The STU2 ballot version was refactored as part of the harmonization of vital records FHIR Implementation Guides by the MITRE corporation, under contract to NCHS. As part of this effort, the IG artifacts were transitioned to FHIR shorthand. The capability statement rendering is provided by the CapStmt liquid template developed by Corey Spears based on original code by Eric Haas.
The editors appreciate the support and sponsorship of the HL7 Public Health Work Group and all volunteers and staff associated with the creation of this resource. The editors appreciate the wisdom and insights provided by the MDI community, including forensic toxicology laboratories, medical examiners and coroners, and jurisdictional vital records departments.
The MDI Community:
The IT vendor community:
Health Level Seven, HL7, FHIR and the [FLAME DESIGN] are registered trademarks of Health Level Seven International, registered in the US Trademark Office. This material contains content from SNOMED CT. SNOMED CT is a registered trademark of the International Health Terminology Standard Development Organization (IHTSDO).
This material contains content from LOINC. LOINC is copyright © 1995-2021, Regenstrief Institute, Inc. and the Logical Observation Identifiers Names and Codes (LOINC) Committee and is available at no cost under the license at https://loinc.org/kb/license/. LOINC® is a registered United States trademark of Regenstrief Institute, Inc.
This guide links terminology directly to the FHIR® Terminology Service for VSAC Resources (Value Set Authority Center (VSAC) - NIH) where applicable using a RESTful API service for accessing the VSAC value sets and supported code systems. It is a requirement of VSAC to log in using your own Unified Medical Language System (UMLS) API Key to view the value sets. See: VSAC UMLS Licensing information.