This page is part of the CARIN Digital Insurance Card (v0.1.0: STU 1 Ballot 1) based on FHIR R4. The current version which supercedes this version is 1.0.0. For a full list of available versions, see the Directory of published versions 
This Implementation Guide was born out of the CARIN Alliance Payer's Implementer Forum where representatives from major health insurance companies in the US come together to collaborate on FHIR server implementation. In 2020, participants of the forum indicated a need for better guidance on how to represent the full data elements found on physical insurance cards within a FHIR-based transaction. In particular, participating payers noted the following challenges when trying to build out FHIR Coverage resources including all the necessary data elements:
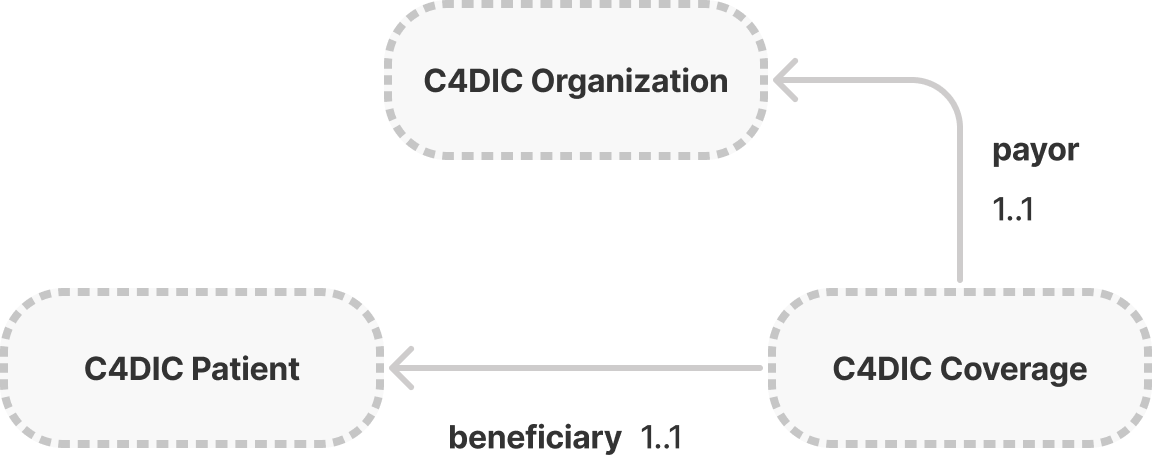
Payers can leverage the Coverage resource, the Organization resource, and the Patient resource to represent the essential information found on the physicial insurance card. The purpose of each resource is as follows:
The below diagram outlines how these resources relate. As shown below, the coverage.payor field will contain a reference to the corresponding Organization resource, and the coverage.beneficiary field will contain a reference to the corresponding Patient resource for the member whose data is being retrieved.
For additional information about the exchange of insurance card information please visit these pages:
This Implementation Guide enables the digital exchange and digital rendering of the elements found on a person’s physical insurance card. The primary use case is to support insurance members who wish to retrieve their current proof of insurance coverage digitally via a consumer-facing application.
This IG does NOT address eligibility checks between health providers and the insurance company.
This IG is not intended to replace use of any existing standards for pharmacy insurance cards, i.e. NCPDP standards, and is being provided to augment existing physical insurance cards where pharmacy benefits may need to be included with other coverage.
In keeping with the 80/20 rule, this IG does not solve for all possible insurance card data elements. If additional data elements of interest are identified by the community, they will be integrated in STU2 of this IG. For example, there are a few unique fields relevant to Medicare cards that were unable to be incorporated into this initial IG development cycle (i.e. CMS Contract Number, PBP Code, Segment ID).