This page is part of the National Healthcare Directory Attestation (v1.0.0-ballot: STU 1 Ballot 1) based on FHIR (HL7® FHIR® Standard) R4. No current official version has been published yet. For a full list of available versions, see the Directory of published versions
This diagram depicts the high-level conceptual design of a central source of national directory data.
Figure 1: National Directory Concept Diagram
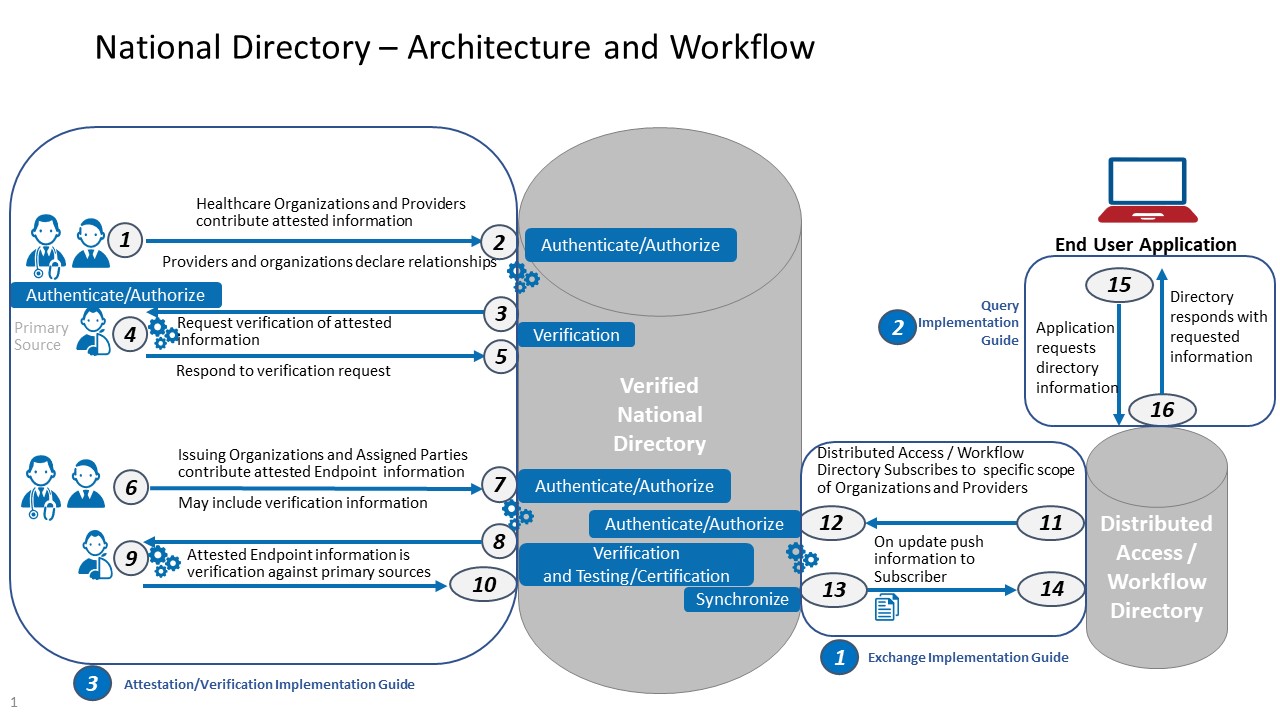
In this diagram, RESTful FHIR APIs facilitate the movement of data into and out of a verified healthcare directory at different points, including:
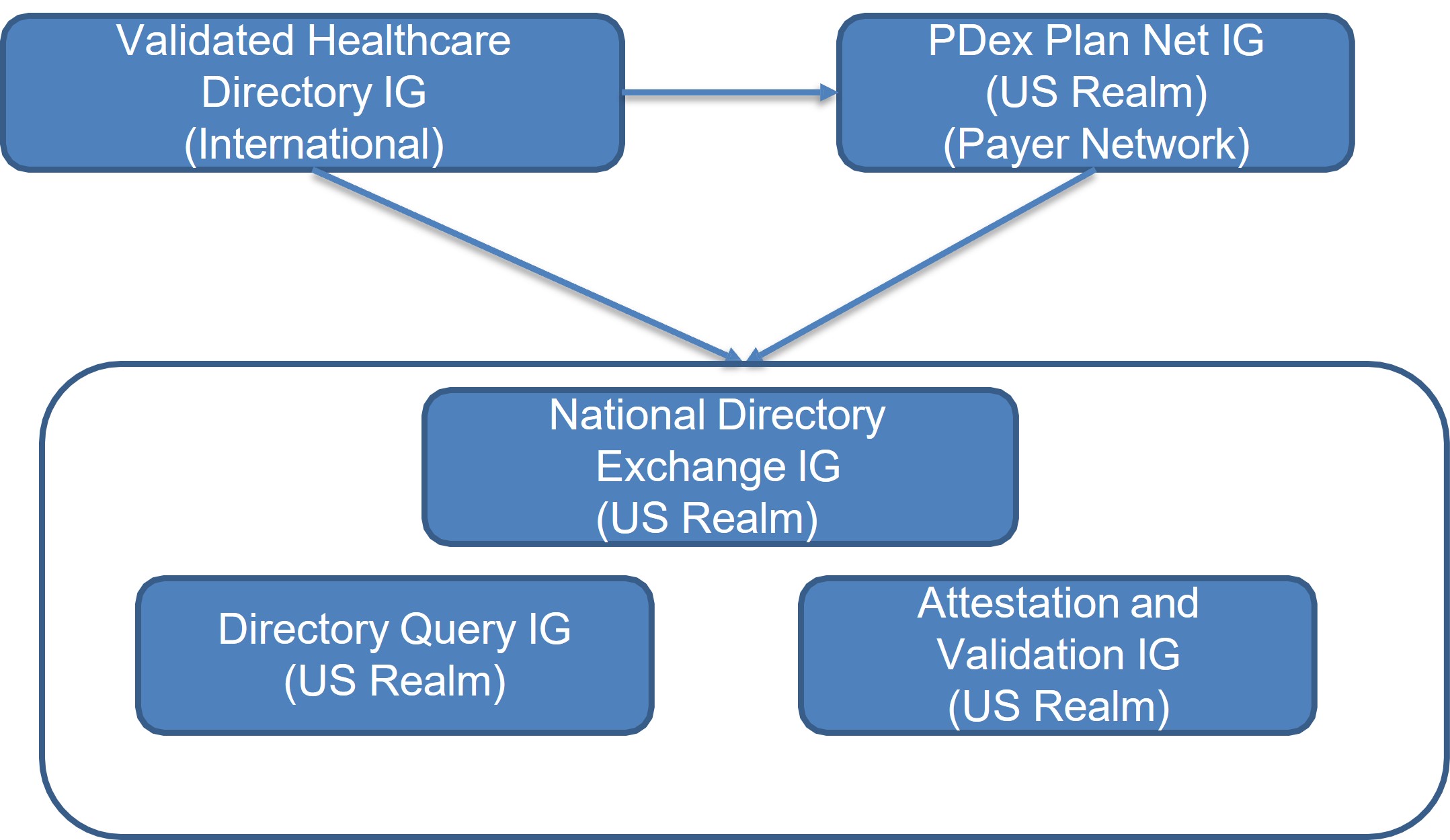
Figure 2: Relationship Between Implementation Guides
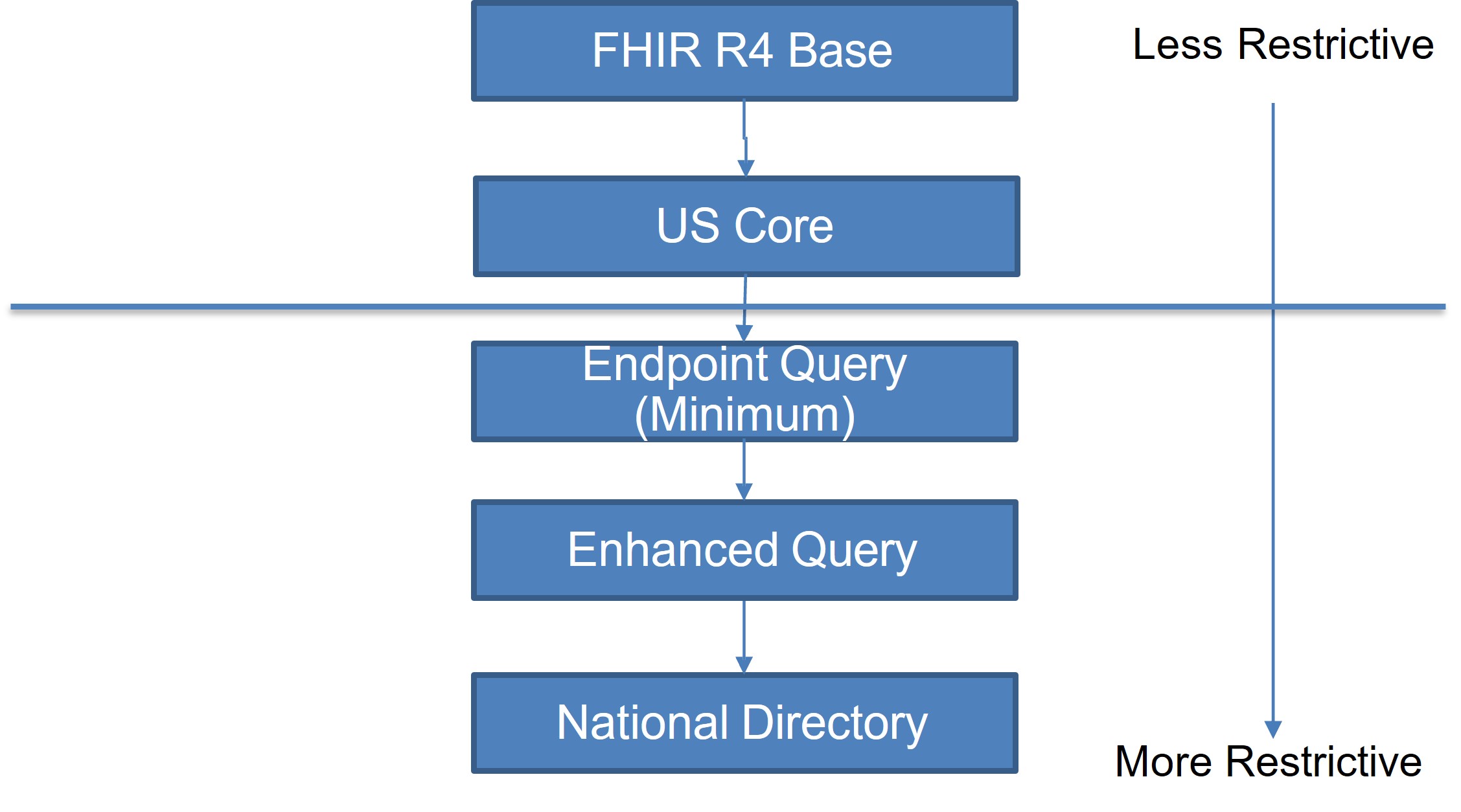
Figure 3: Profile and Extension Inheritance Between Implementation Guides
Attestation describes the process by which authorized entities submit information about themselves, their roles, their relationships, etc. for inclusion in a healthcare directory.
Guidance in this section is primarily intended to describe expectations for implementers using a FHIR API to manage attestation. An implementer’s unique implementation context, including local business needs, applicable laws/regulations/policies, usability considerations, etc. will determine an implementer’s approach to many of the attestation considerations described in this section. As we do not anticipate every implementer will use the same approach to attestation, we have not provided a set of attestation profiles or defined an attestation API. Implementers SHALL make any attestation requirements, including but not limited to profiles and/or API documentation, available to any stakeholders involved in the attestation process.
We acknowledge that implementers may use processes other than a FHIR API, such as paper-based forms, to obtain attested data. Such processes are considered out of scope for this guide.
This guide covers multiple attestation scenarios:
Each of these scenarios may encompass different sets of “permitted” data. For example, an individual provider attesting to her own information may not have the right to also attest to information about an organization she works for. These “rights” are assigned by each implementation of a verified national directory, and can help prevent the submission of duplicate records. In general:
Additionally, implementers may set requirements for the minimum amount of data different groups of stakeholders must attest to. For example, a US implementation might require all licensed providers to attest to their National Provider Identifier (NPI). In general, implementers might specify different minimum attestation requirements across three classes of stakeholders:
We expect stakeholders will typically use a SMART on FHIR application to help attesters manage the attestation process (i.e. to submit attested data in the form of FHIR resources via a RESTful API). Such an application may be offered by an entity maintaining a verified healthcare directory, an application authorized by the verified healthcare directory or owned by the stakeholder(s) submitting attested data.
Before accepting attested data, a verified healthcare directory should have policies to ensure:
Once these preconditions have been met, a typical attestation workflow might involve:
The FHIR specification describes multiple approaches for managing interactions over an API, including:
This implementation guide is not prescriptive about which approach(es) a verified healthcare directory should use to manage attestation. However, as any attestation will likely involve the submission of multiple FHIR resources representing information about one or more attesters, transaction Bundles can alleviate the need for more complex logic to manage referential integrity in attested information.
Implementations relying on individual API interactions or batch Bundles may have to specify an “order of operations” to ensure attested data can be successfully submitted to the verified healthcare directory server. For example, as a general guideline, resources may need to be submitted in the order of:
Depending on the context of implementation, the entity maintaining a verified healthcare directory may have to manage record collision or duplication (i.e. multiple attesters attempting to simultaneously submit updates to the same record, or multiple attesters attempting to attest about the same set of information).
The FHIR specification provides some guidance on managing collisions using a combination of the ETag and If-Match header in an HTTP interaction. We recommend verified healthcare directory implementers use this approach.
To manage duplicate records, we generally recommend that verified healthcare directory implementers define a robust verification process with policies for identifying and resolving duplicates. Any additional technical capabilities are beyond the scope of this implementation guide.
The verified national directory performs a validation process to check the general structure, content, etc. of the submission (e.g. checking consistency w/data type, required elements are present, references to existing resources are correct, codes are from appropriate value set etc.). Validation is critical for ensuring that users of a healthcare directory can rely upon the data in the directory. Validation can refer to separate but related processes: validation of FHIR resources (e.g. checking consistency w/data type, required elements are present, references to existing resources are correct, codes are from appropriate value set etc.). Validation includes (but is not limited to) testing conformance to:
Verification is critical for ensuring that users of a healthcare directory can rely upon the data in the directory as being accurate, not just meeting a technical specification.
Implementers will typically determine how primary source verification occurs operationally, based in part on the capabilities of the primary sources used for verification. For example, a primary source may already offer a mechanism like an API for verification content against its records. In other cases, an implementer may want to define an API that the primary source can access to push and/or pull content related to verification. Implementers may also consider less technical approaches, such as manual verification, or more stringent requirements, such as mailing a postcard to confirm an address.
Certain types of data may have different verification requirements. For example, verification of a relationship might require confirmation from each stakeholder participating in the relationship. Some data may have to be verified more frequently (e.g., license status), while other data can be verified once (e.g., education history) or not at all (e.g., a provider’s spoken language proficiency).
As with attestation, we expect National Directory implementers may use different approaches to verification. This guide provides profiles for a small number of suggested verification APIs. Implementers SHALL make any verification requirements, including but not limited to profiles and/or API documentation, available to any stakeholders involved in the verification process.
This implementation guide includes a profile for the VerificationResult resource for representing information about validation and verification. The VerificationResult resource includes a number of data elements designed to record information pertaining to the verification processes defined by implementers, as well as the outcome of verification for a specific data element/set of elements/resource. The verification profile includes data elements describing:
Verification may occur on the total contents of a resource, a collection of elements in a resource, or a single element. Any entity with access to a data element in a verified healthcare directory SHOULD also have access to any verification information pertaining to that element.
Verification Methods
We envision a verified national directory as a public or semi-public utility and make a significant portion of the information openly available. However, a verified national directory may include sensitive data that is not publicly accessible or accessible to every verified healthcare directory stakeholder. For example, an implementer might not want to make data about military personnel, emergency responders/volunteers, or domestic violence shelters available to everyone with access to the verified healthcare directory, or to users in a local environment who have access to data obtained from a verified healthcare directory.
We expect that a verified national directory operational policies and legal agreements will clearly delineate which data stakeholders can access, and if necessary, require stakeholders to protect the privacy/confidentiality of sensitive information in downstream local environments. As such, we have included a Restriction profile based on the Consent resource to convey any restrictions associated with a data element, collection of elements, or resource obtained from a verified healthcare directory.
Although FHIR resources define discrete business objects, related resources may have similar data elements. For example, the HealthcareService, PractitionerRole, and Location resources all include data elements describing availability. In some circumstances, values in these common data elements may not align across resources, potentially creating ambiguity. For example, in this IG, a Location resource might indicate that the location no longer accepts patients. However, a PractitionerRole resource for a provider working at the location might indicate that the provider is accepting patients (e.g., by referral only). In some cases, these inconsistencies are valid representations of the complexities of healthcare systems. In others, data might have been entered in error, outdated, or otherwise inaccurate.
The FHIR specification does not provide guidance on managing common elements across resources to reduce redundancy or ambiguity. Likewise, this implementation guide does not provide additional guidance. Implementations should consider further constraining profiles, creating invariants, or requiring data sources (e.g., attesters) to contribute data in a consistent format. Some resources include elements for describing exceptions, such as the AvailabilityExceptions field on HealthcareService, Location, and PractitionerRole. Additionally, verification processes may help discover and address inconsistencies across resources.