This page is part of the Da Vinci Value-Based Performance Reporting Implementation Guide (v1.1.0: STU1.1) based on FHIR (HL7® FHIR® Standard) R4. This is the current published version. For a full list of available versions, see the Directory of published versions
| Page standards status: Trial-use |
There are three profiles specified in this version of the implementation guide:
evaluatedResource references the VBP Quality MeasureReport profile. This profile derives from the Da Vinci Data Exchange for Quality Measure IG's DEQM Summary MeasureReport profile and provides additional capability to support the need for exchanging quality measure data relevant for value-based performance reporting.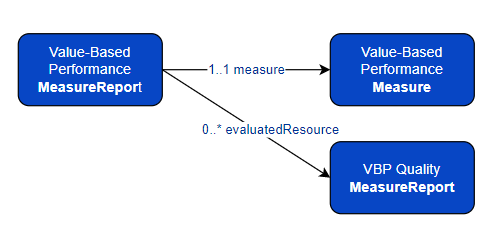
Figure 2-2 describes value-based performance reporting workflow between a Payer and a Provider. Payer creates Value-Based Performance Measure for a value-based contract and generates VBP MeasureReport for a performance period, Provider then periodically gets the reports from the Payer.
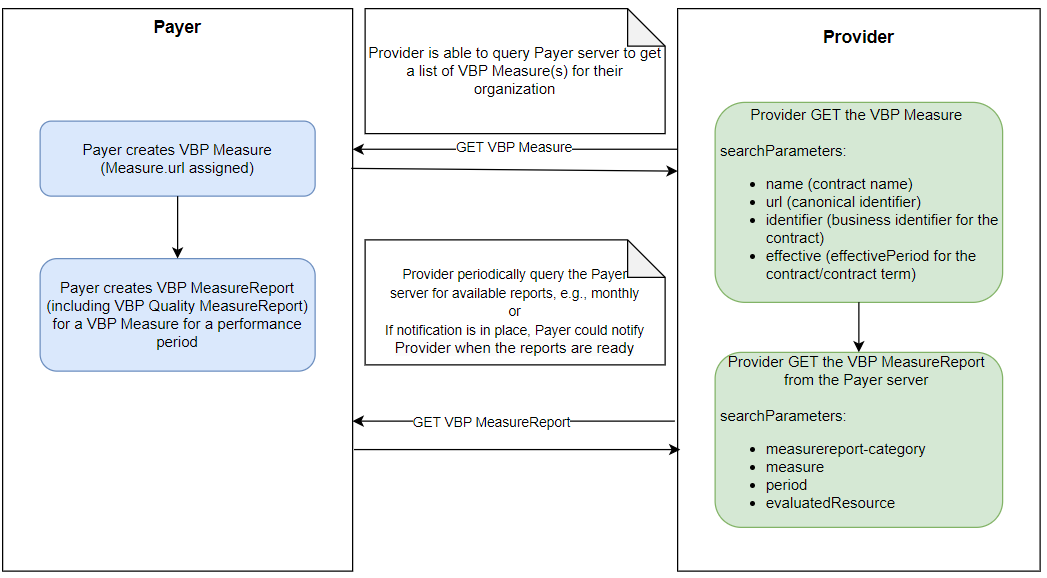
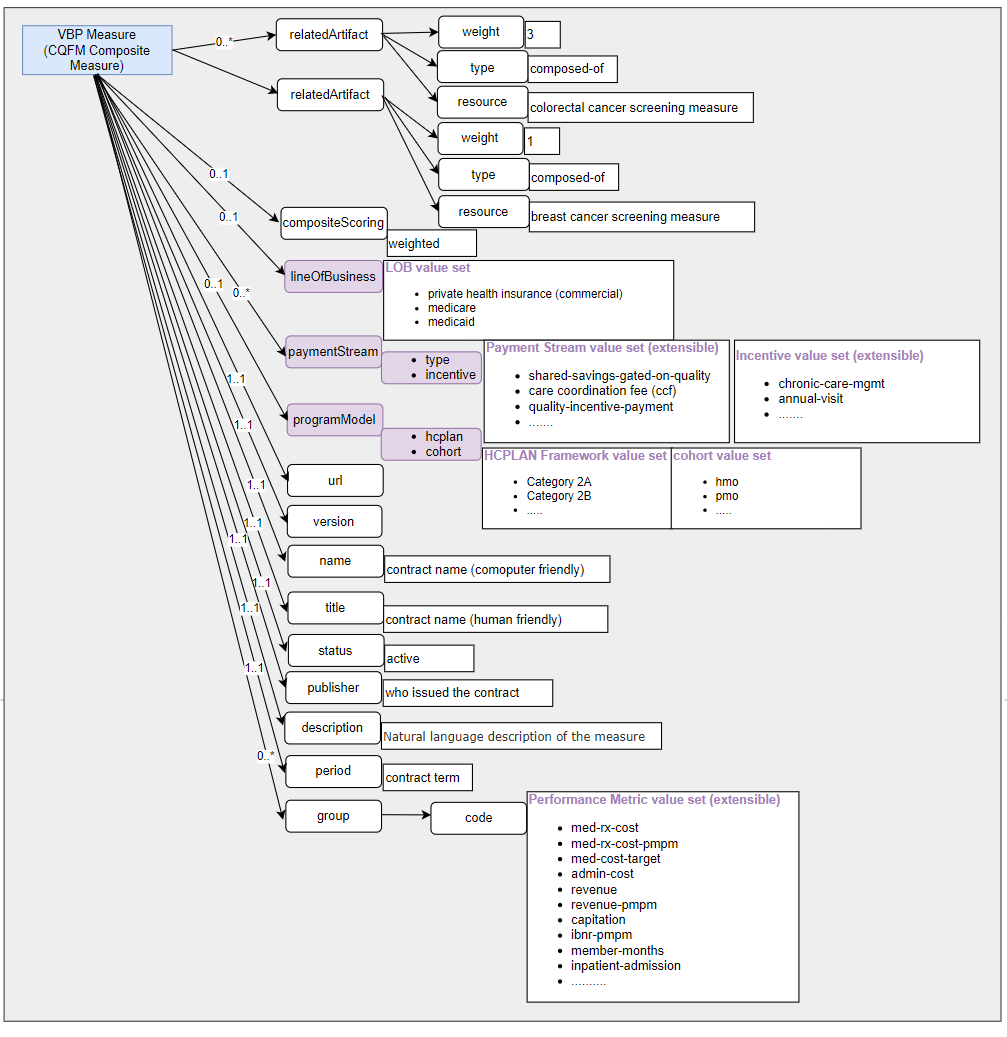
Value-based payment models are expected to grow across all lines of business. The adoption of value-based care has accelerated in recent years, and this trend could continue in the coming years as payers, employers, and the government embrace these value-based care models. Value-based contracts encompass a broad variety of models, such as capitation, pay-for-performance, pay-for-quality, and shared savings to name a few. The performance metrics and measures that these value-based contracts need to measure and to track are also very broad, which spans over financial, quality, utilization and more. Because of the challenges with ever-expanding value-based payment models and performance metrics associated with those models, it would be near impossible and unsustainable to specify a comprehensive list of named representations for these different value-based care models and metrics. This implementation guide has taken the approach of defining a framework for value-based performance reporting. The profiles specified in this implementation guide provide standard structural representation that is intended to support reporting on various value-based payment models. Commonly used payment models and performance metrics are defined in value sets with extensible binding, which provides Payer and Provider the flexibility for reporting value-based payment models and metrics that are not yet defined in this implementation guide or those that are applicable only to their own organizations.
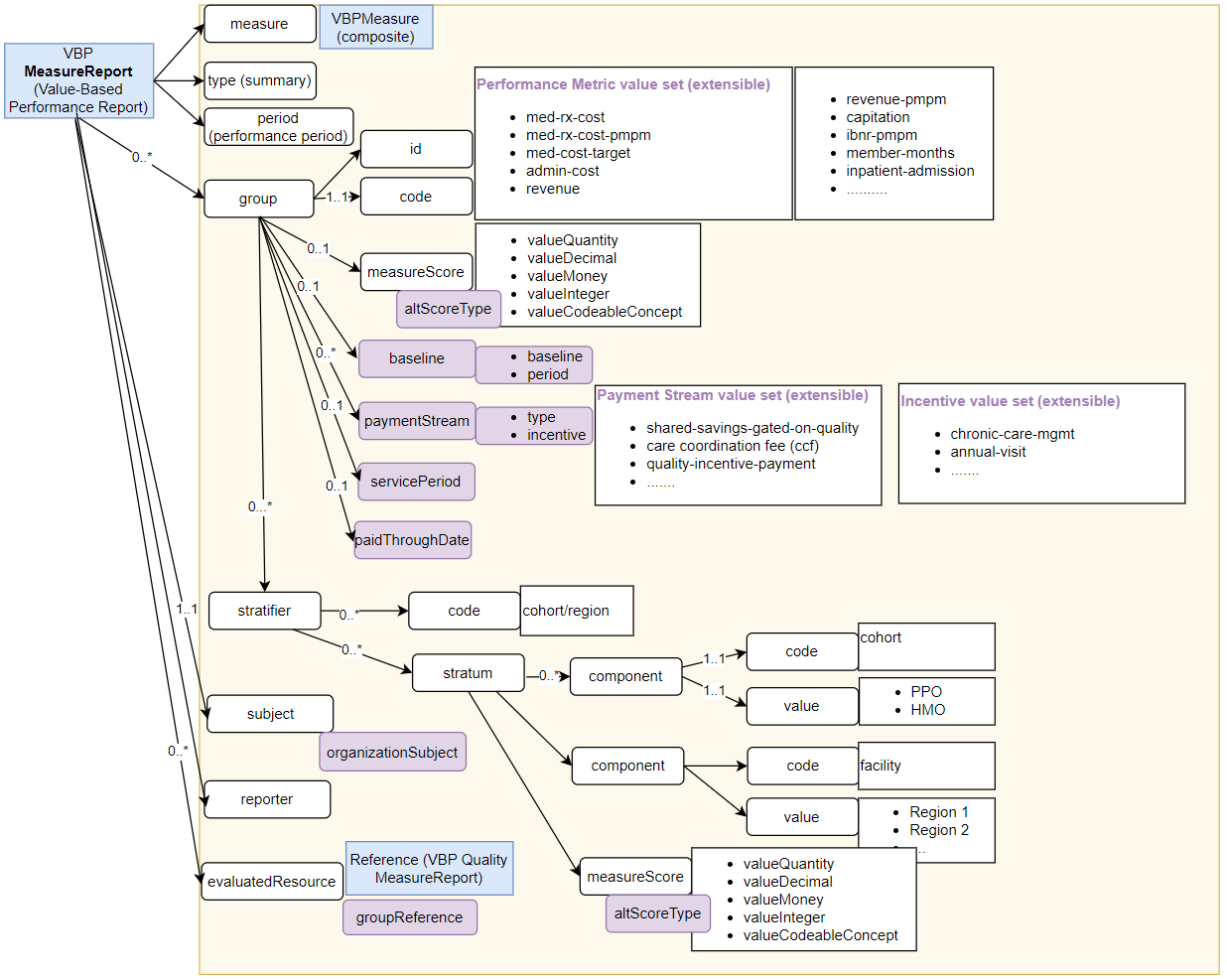
The Value-Based Performance MeasureReport (VBP MeasureReport) is a profile on the MeasureReport resource. Each MeasureReport.group corresponds to a performance metric.
MeasureReport.group.code has an extensible binding to the Performance Metric value set. This value set contains a list of commonly used performance metrics for various value-based payment models. Several extensions are added to the group element to provide additional information about a performance metric.measureScore is the value of a performance metric. An extension Alternate MeasureScore is added to allow additional data types including decimal, integer, CodeableConcept, boolean, and Money to be used in addition to Quantity.paymentStream is a complex extension. The type is required, which has an extensible binding to the Payment Stream value set. The Payment Stream value set defines commonly used value-based payment models such as care coordination fee, shared savings percent, shared savings gated on quality, and etcetera. The incentive is an optional field and is intended to provide more granular incentive program information for the Quality Incentive Payment payment stream, such as chronic care management and annual office visit. The paymentStream has cardinality of 0..*. It is possible for a performance metric to be associated with different payment streams.baseline is a complex extension. The baseline value of the performance metric and the time period the baseline was measured could be provided.servicePeriod is the service period for a performance metric. Each performance metric may have a different service period.paidThroughDate is the ending date of the pay cycle.Value-based performance reports often include data on performance on overall population and stratified results on those performance metrics based on variety of stratifiers. This IG has defined a list of stratifier codes, which include facility, taxid, group, geography, and cohort.
MeasureReport.group.stratifer provides the capabilities of stratifying based on a single stratifier or combination of a number of stratifiers.stratifier.stratum.value would be selecting from a list of codes that represent the regions. The exact codes may be specific to a payer or provider organization.stratifier.stratum.component.Many value-based payment models involve quality. The implementation guide reuses the Data Exchange for Quality Measure (DEQM) Summary MeasureReport for reports on quality measures. The VBP MeasureReport profile created a slice on the MeasureReport.evaluatedResource to reference the VBP Quality MeasureReport profile, which is derived from the DEQM Summary MeasureReport. The groupReference extension allows a VBP MeasureReport to be linked to a specific performance metric by using the group.id if needed.
For a value-based performance report, the subject of the report is a reference to the ATR Group profile defined in the Da Vinci Member Attribution (ATR) List IG. ATR Group is a Member Attribution List that contain information related to the members who are attributed to a value-based contract.
Figure 2-2 provides a structural overview of the VBP MeasureReport. (Note: elements that are added as extensions are indicated with purple background.)
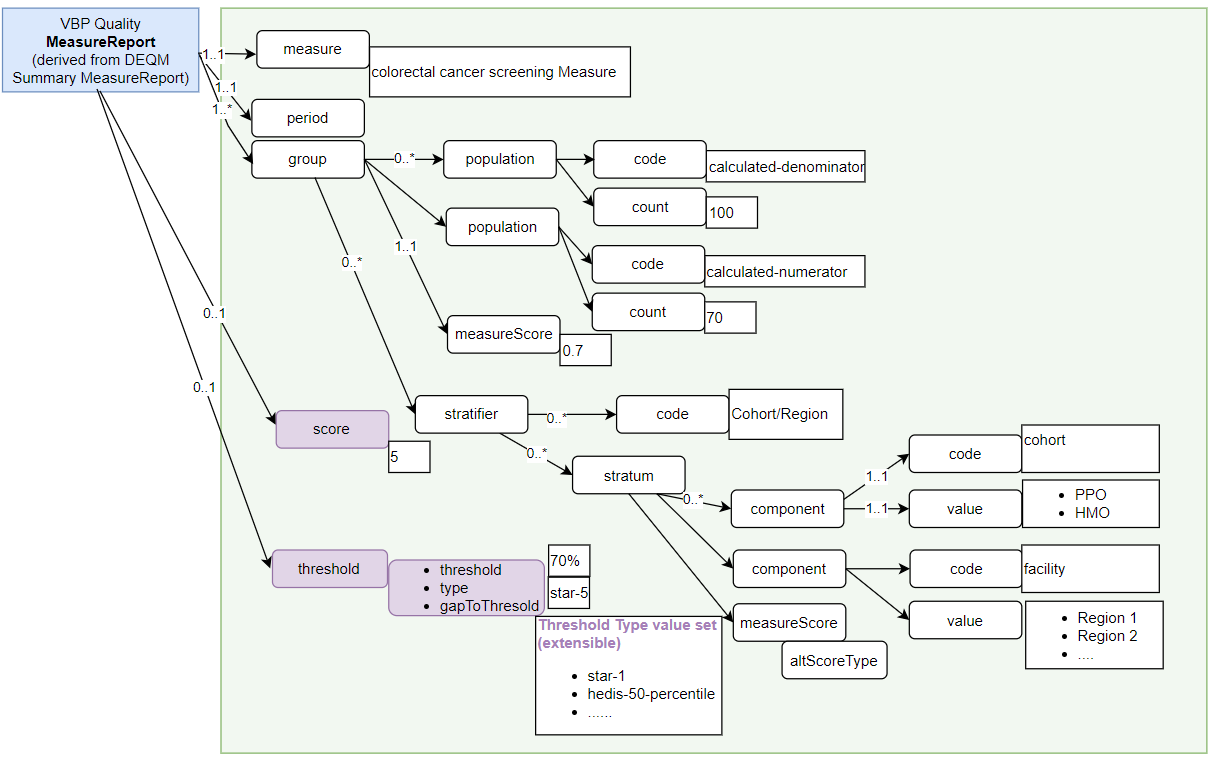
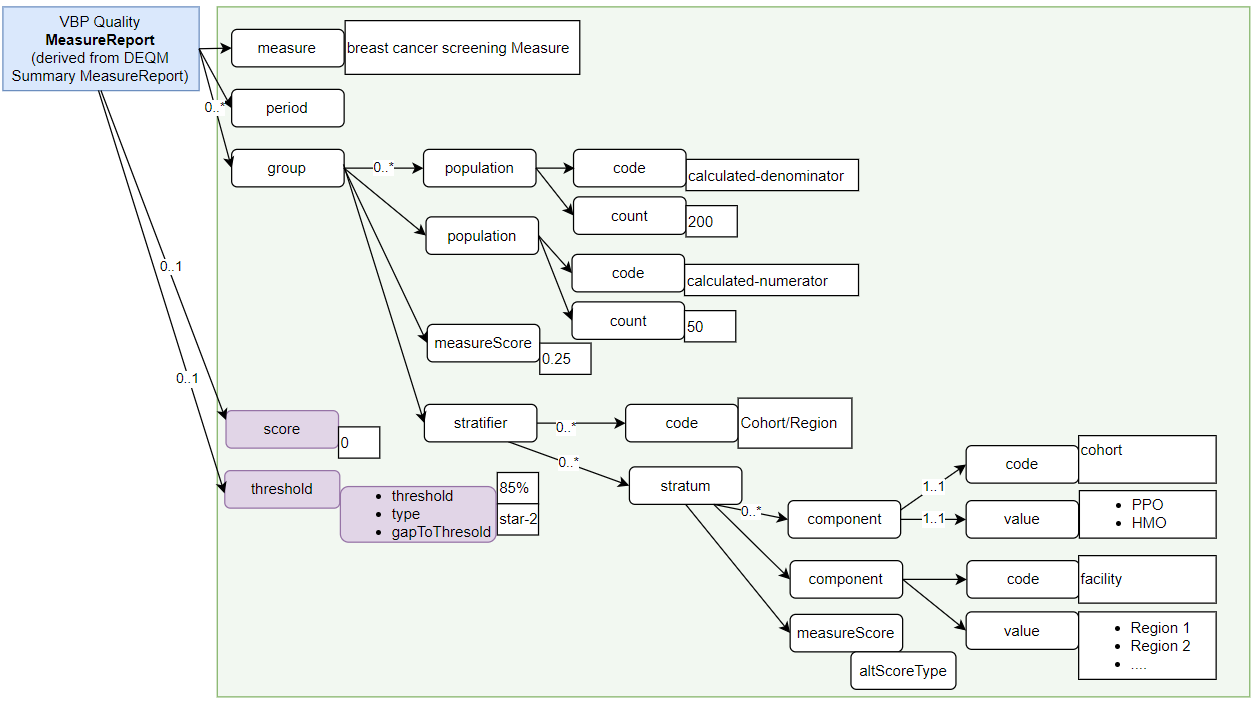
VBP Quality MeasureReport is based on the DEQM Summary MeasureReport with a few extensions.
MeasureReport.threshold: value-based performance reports often include threshold information for a measure, for example, the threshold for this measure for a 4 star in a star rating is 85%. The type indicates what kind of threshold. The threshold is the value of the threshold, such as 85%. The gap that needs to meet the threshold can be represented using the optional gapToThreshold.MeasureReport.score: this score is used to represent scores such as a star rating score.This profile has defined a VBP Measure Population Type value set. This value set added two new codes calculated-denominator and calculated-numerator to the Measure Population Type value set from the base Measure resource. The calculated-denominator is the resulting denominator when calculating performance rate, for a proportion measure, this would be the result of denominator – denominator exclusion – denominator exception. Same applies to the calculated-numerator.
Figure 2-3 and Figure 2-4 used the colorectal cancer screening and the breast cancer screening measures as examples to illustrate the use of the VBP Quality MeasureReport.
The VBP Measure is used to represent value-based contract information that are needed for value-based performance reporting.
This profile added a few extensions to represent the following: