This page is part of the Da Vinci Value-Based Performance Reporting Implementation Guide (v1.0.0-ballot: STU1 Ballot 1) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 1.1.0. For a full list of available versions, see the Directory of published versions
| Official URL: http://hl7.org/fhir/us/davinci-vbpr/ImplementationGuide/hl7.fhir.us.davinci-vbpr | Version: 1.0.0-ballot | |||
| Active as of 2023-07-31 | Computable Name: ValueBasedPerformanceReporting | |||
The Da Vinci Fast Healthcare Interoperability Resource (FHIR) Value-Based Performance Reporting (VBPR) Implementation Guide supports exchanging financial and quality performance data based on contractual performance measurements agreed to by payers and providers.
Value-based contracting is important to the US healthcare system for several reasons:
Reporting performance against the specific details of a contract may include financial, quality, utilization, etc. over defined time periods. This timely performance reporting provides the needed transparency required at the point of care and is essential to the success of value-based contracts for both payers and providers.
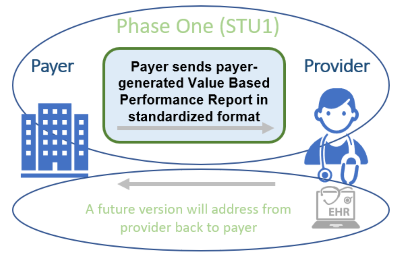
The first Standard for Trial Use (STU) version of this implementation guide focuses on the standard exchange format of value-based financial and quality performance reports for payers to providers. It may also benefit both providers and payers by reducing the administrative burden to providers by standardizing the reporting they receive across all payers.
This implementation guide is supported by the Da Vinci initiative which is a private effort to accelerate the adoption of Health Level Seven International Fast Healthcare Interoperability Resources (HL7® FHIR®) as the standard to support and integrate value-based care data exchange across communities. Like all Da Vinci Implementation Guides, it follows the HL7 Da Vinci Guiding Principles for exchange of patient health information. As an HL7 FHIR Implementation Guide, changes to this specification are managed by the sponsoring Clinical Quality Information (CQI) Work Group and are incorporated as part of the standard balloting process.
This implementation guide is divided into several pages which are listed at the top of each page in the menu bar:
Value-Based Performance Reporting (VBPR) offer insights into the performance of healthcare providers and organizations by evaluating their financial, quality, cost, and efficiency aspects. These reports play a crucial role in assessing and comparing providers within value-based contracts. The objective of such contracts is to encourage superior care, enhance patient outcomes, and lower costs by compensating providers according to their performance, as opposed to the quantity of services provided.
Payer-generated performance reports are crucial because payers are generally the arbiters in determining financial performance on risk contracts with health systems. Many times, payers have the best source of information on Per Member Per Month (PMPM) spend, contractual terms, regional or historical trends, and other financial information that health systems need to track and manage performance on those contracts. Claims data is important but insufficient on its own because state and federal requirements mask certain types of data that make accurate financial calculations difficult.
Healthcare providers and participating organizations submit performance data, including quality measures, cost, and utilization metrics, to payers or other regulatory bodies for evaluation and analysis. There have been numerous value-based performance initiatives launched by both public and private payers, including accountable care organizations (ACOs), bundled payments, and pay-for-performance programs to name a few. These initiatives have continued to evolve and expand, with a growing emphasis on patient-centered care, population health management, and the use of data analytics to drive quality improvement and cost containment.
Value-based performance reports are generated by payers to summarize provider performance across different categories, including lines of business, contracts, populations, quality measures, and financial metrics and reporting periods on a scheduled and ad-hoc basis.
Based on the calculated performance scores, incentive payments are calculated and distributed to providers as rewards or penalties, encouraging continuous improvement in care quality and efficiency.
HCP-LAN (Health Care Payment Learning and Action Network)1 is a public-private partnership established in 2015 by the US Department of Health and Human Services (HHS) to accelerate the transition to value-based payment models in the US healthcare system. HCP-LAN has defined several categories that help to categorize the alternative payment models (APMs).2, 3 These categories are intended to provide a framework for evaluating the complexity and risk associated with different APMs, and to help stakeholders understand the trade-offs between different payment models.
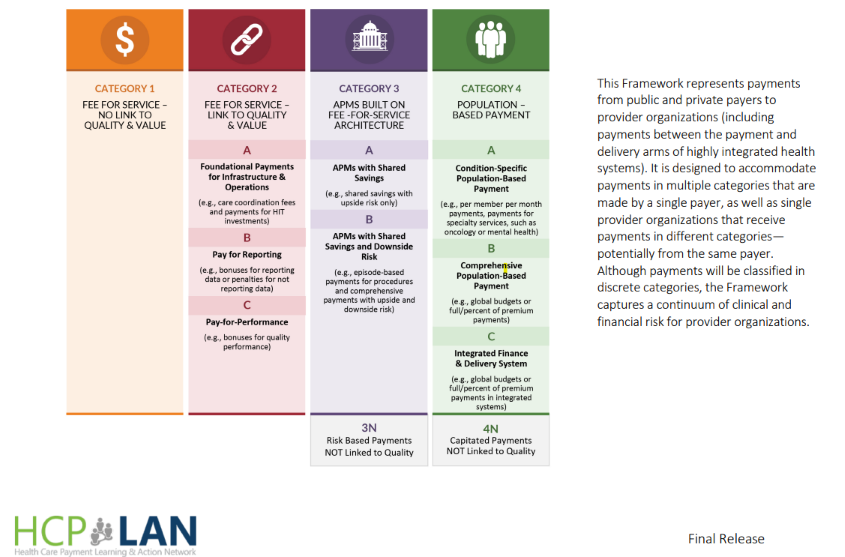
Category 1: Fee-for-Service with No Link to Quality and Value: This level includes traditional fee-for-service payment models that do not provide incentives for quality improvement or cost containment. (Note that Category 1 is not addressed in this implementation guide).
Category 2: Fee-for-Service with Links to Quality and Value: foundational payments for infrastructure and operations, pay for reporting, or shared savings.
Category 3: APMs build on fee-for-service architecture: This level includes payment models that focus on upside risk only or that episode-based payment for procedures and comprehensive payments with upside and downside risk. This category also included risk-based payments NOT linked to quality.
Category 4: Population-based Payment: This level includes payment models where providers receive a fixed payment for a specific population, such as a patient panel, and are responsible for delivering all necessary care within that population. This category also includes global budgets or full/percent of premium payment and integrated finance and delivery system. This category also includes capitated payments not linked to quality.
While a framework is in place to identify the types of value-based agreements payers and providers can participate in, there is a challenge in collecting, analyzing and reconciling the numerous reports providers receive from payers. Some of these challenges include:
The goals of implementation guide are:
The initial phase of this implementation guide focuses on:
Future versions of this implementation guide may include functionalities to support topics such as:
This implementation guide was made possible by the thoughtful contributions of the following people and organizations:
The Da Vinci Project member organizations.