This page is part of the Documentation Templates and Rules (v1.1.0-ballot: STU 1.1 Ballot 1) based on FHIR R4. The current version which supercedes this version is 1.0.0. For a full list of available versions, see the Directory of published versions 
A Payer is an entity who pays for the service of providers. The majority of payers here are also referred to as health insurance companies.
The payer IT system SHALL be the primary system responding to DTR queries.
In this specification payer rules are CQL statements used in a provider context to facilitate meeting documentation requirements.
A healthcare provider organization contains medical providers such as hospitals, doctors, etc.
The Electronic Health Record (EHR) system shall be the primary system used to initiate the DTR process. The SMART App Launch will typically be initiated from within the EHR.
The goal of DTR is to collect clinical documentation and/or to encourage the completion of documentation that demonstrates medical necessity for ordered items or services.
It is possible to have a process where the focus is on the interaction with the EHR and an external application. Examples of external systems are administrative, payment, practice management, scheduling, and other applications.
If information required to complete the Questionnaire is not available to the SMART on FHIR application, then the application will need to prompt the provider to enter the missing information. Ultimately, the solution is to provide greater integration between the EHR and other supporting applications. (e.g., Quality measures may also require this type of integration)
Electronic Health Record (EHR) is used in this IG and can be considered equivalent to Electronic Medical Record (EMR) or a Practice Management System (PMS).
Within DTR, the SMART on FHIR app (or equivalent native EHR app) serves as a middleware layer easing payer and provider integrations. This functionality enables DTR to gather Questionnaire resources, retrieve FHIR resources from EHRs, and run rules (CQL) to reduce the time involved in looking up documentation requirements.
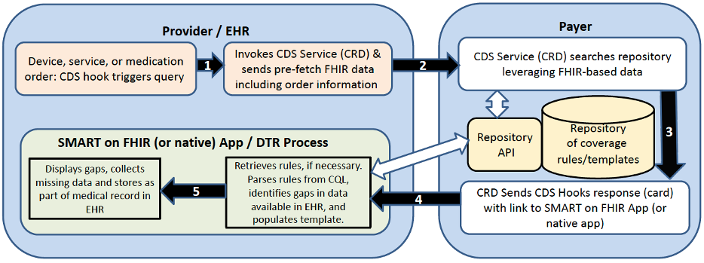
The Coverage Requirements Discovery (CRD) service portion of the workflow is responsible for verifying with the payer a given item, certain medications, procedure or other service requires documentation and/or Prior Authorization. It then provides the necessary links for the app to be launched and run. In most cases, the CRD service will return a CDS card populated with an app launch link for the DTR process, a link to a resource, and a DeviceRequest, MedicationRequest, or ServiceRequest resource ID. The app launch link can be used in a user interface in order to launch the app. While CRD may verify that documentation and/or prior authorization is required, it does not manage completion of documentation, prior authorization, or validation of rules.
The DTR process is responsible for accessing Questionnaire resources and rules (CQL), hen prepopulating the questionnaire with EHR data and finally checking if the available EHR data satisfies requirements, as well as allowing for the manual population of any missing data.
The graphic shows a high-level overview of CRD and DTR (DTR is the SMART on FHIR app or equivalent native EHR app)
Note: This workflow is just one example used to help illustrate the CRD and DTR APIs. It is expected that a supplemental guide will be produced moving forward to help implementers with more concrete examples.
As an example, a clinician might order, “Home Oxygen Therapy”
This example shows an overview of how the DTR SMART on FHIR app (or equivalent native EHR app) fits into a workflow when ordering Home Oxygen Therapy.
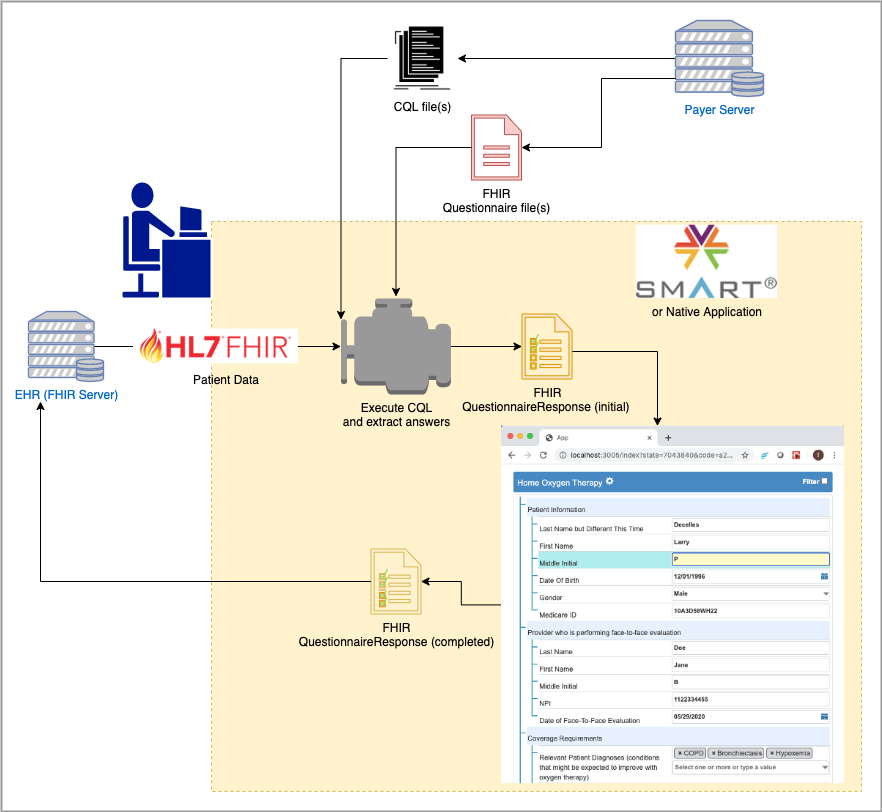
There is no need for the user to see the Questionnaire if it can be auto completed, unless they need to approve sending the result to the payer or to sign the information prior to submission. The application SHALL give the provider the ability, but not the requirement to review any information prior to sending it to a third party. This ability may be turned-off by the organization and possibly the individual provider.
Questionnaires SHALL indicate which items are necessary using the
requiredproperty, and the application should use that property to decide when a Questionnaire has been sufficiently auto completed.
If the resulting information is to be sent to a third party (e.g., payer), the DTR SMART on FHIR App (or equivalent native app) SHOULD include a configurable step to allow the provider to review and grant permission to send the information gathered in the QuestionnaireResponse before sending.
However, this SHOULD be configurable on a site or provider basis.
If the resulting information is to be sent to a third party (e.g., payer) see Section 4.4.5.1
DTR does not support creating new orders or changing existing orders. DTR supports documentation requirements for device, service, and medication requests. When the required documentation cannot be populated from the EHR, DTR provides the ability to capture the missing information.