This page is part of the Da Vinci - Member Attribution (ATR) List (v0.1.0: STU 1 Ballot 1) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.1.0. For a full list of available versions, see the Directory of published versions
Providers need to access Member Attribution Lists for the following business needs
Performing end of year reconciliation to get ‘credit’ for the right patients based on plans/contracts.
Monthly membership tracking to see trends and confirm accountable care PMPM payments
Project membership for upcoming year based on prospective lists at end/start of year.
Keep historical data of patients for continuity of care as members fall off or get added to the list
Use the list to close care gaps for members that ‘count’ in financial reconciliation
Use the list for performance reporting on specific targets and measures.
Use the list to identify patients that they can work on to improve performance for specific measures and targets.
Using FHIR based APIs, providers and payers can exchange Member Attribution Lists which can enable existing business processes and systems to meet the above business needs. The creation of a Member Attribution List typically starts with a need to identify the patients for a specific purpose such as Risk Based Contracts, Quality Reporting. Once the patients are identified other FHIR APIs and Davinci specifications can be used to retrieve clinical, financial or other relevant information as needed.
Provider Organization A enters a risk based contract with Payer B. As part of establishing the contract targets, specific measures, financial incentives are documented. Payer B uses historical claims and other information present about members to create a Member Attribution List for Provider Organization A. The Member Attribution List identifies the list of patients that Provider Organization A is responsible for as part of the contract. Payer B needs to exchange this list with Provider Organization A periodically to ensure that Provider Organization A is aware of the list of patients that it is responsible for as per the contract. Payer B could publish the list in standard way and Provider Organization A retrieves the list for use. Alternatively Provider Organization A may request for the list and Payer B provides the list once it is ready.
Provider Organization A enters a risk based contract with Payer B. As part of establishing the contract targets, specific measures, financial incentives are documented. Payer B uses historical claims and other information present about members to create a Member Attribution List for Provider Organization A. The list is published by Payer B and Provider Organization A retrieves the list. Once Provider Organization A reconciles the list, it identifies a list of changes that need to be done to the list and notifies the Payer B about the changes. Payer B either accepts or rejects the changes and may modify the existing Member Attribution List. If the list is modified, Payer B notifies Provider Organization A of the changes. Provider Organization A retrieves the list and starts using the list for various business needs.
** Note: For the initial version of the Implementation Guide, the notification of changes and requesting changes are not in scope. These aspects will be examined in future releases.
The following definitions will be used to document the various workflows encountered during Member Attribution List exchange.
Attribution: Results of Algorithmic process that assigns patients to providers or payers or Groups. Assignment process where patients are just assigned to the group manually. A Patient could declare to be part of a Group by providing or selecting their PCP information or ACO information.
Add examples for each of the above - For example when patients belong to a HMO plan there is an Attribution List created with all the patients who are on the HMO plan.
Member Attribution List: Enumeration of patients who are attributed to payers, providers, medical homes or groups. The Attribution list contains the patient information along with information such as Attributed Provider, Health Plan information, Validity Period for the list, Risk Information etc.
Attributed Provider: Provider responsible for the health of the Patient per the contract and will receive the payments and credits based on performance.
Producer: Entity creating the attribution list. Owns the master copy of the list Allows for changes to be made to the list Can receive an initial list from consumer and owns the list after that and publishes the list from that point
Consumer: Entity consuming the attribution list May contribute to the creation of the list of the Producer May request changes to be made to the list published by the Producer Can receive an initial list from producer and can request changes after that point in time
Attribution List Data: Data contained within the attribution list. Data includes
Attribution List Changes: Addition of patients to the attribution list Deletion of patients to the attribution list Changes in attribution list data
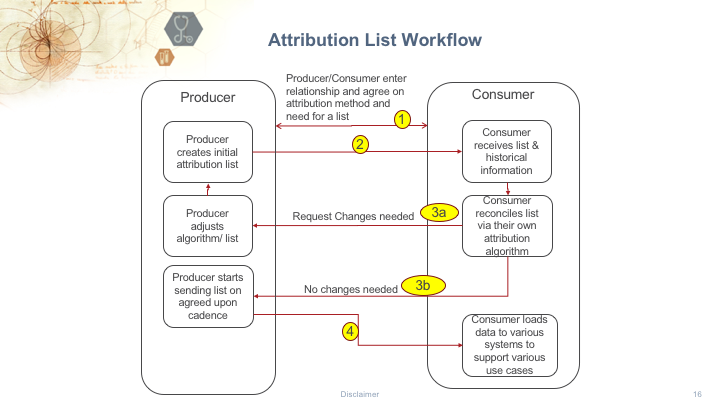
The following is a brief description of the workflow steps with a Payer representing the Producer and a Provider Organization representing the Consumer.
**1. Payer (Producer) and Provider (Consumer) enter into a contract **
Provider and a Payer enter into a contract with specific terms and conditions and decide on the need for a Member Attribution List. Payer internally creates the Member Attribution List using internal processes and existing data about the patients.
**2. Payer (Producer) Informs Provider (Consumer) and makes the List available to the Provider **
In this step the Payer informs the Provider about the list and makes it available to the Provider. The specific mechanism of how this exchange happens varies based on Payers and Providers. This implementation guide will specify standards for this interaction.
**3a. Provider (Consumer) informs Payer (Payer) about changes **
Once the Provider receives the list in Step 2, Provider reconciles the list with internal lists and data and in case changes are needed, notifies the Payer about specific changes. These changes could be to add additional patients, remove patients from the list etc. The specific mechanism of how this exchange happens varies based on Payers and Providers. Future versions of this implementation guide will specify standards for requesting and notifying of changes.
**3b. Provider (Consumer) informs Payer (Producer) about no changes **
Once the Provider receives the list in Step 2, Provider reconciles the list with internal lists and data and in case no changes are needed, notifies the Payer about finalizing the list. The specific mechanism of how this exchange happens varies based on Payers and Providers.
**4. Payer (Producer) makes list available to Provider (Consumer) at regular intervals **
Once the list is finalized, the Payer and Provider agree to exchange the list periodically as required. The specific mechanism of how this exchange happens varies based on Payers and Providers. This implementation guide will specify standards for this interaction.
NOTE: The above workflow is the normal scenario. In addition to the above workflow the Producer may change the list periodically based on additional data. As this happens the Producer may decide to redo Steps 2 through 4.
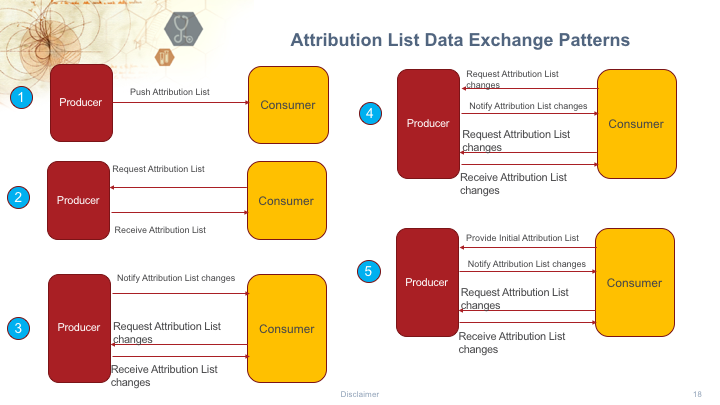
The section takes the workflow described above and identifies the different types of exchange patterns that are currently used. Although each of the patterns identified below are used in the real world, the initial version of the Implemetnation Guide will focus on the exchange mechanisms identified in pattern #2.
</br>
The following are brief descriptions of the Member Attribution List Exchange patterns.
Pattern 1: In pattern 1, the Producer is pushing the list to the consumer using a “One-way push” exchange pattern.
Pattern 2: In pattern 2, the Consumer request the Member Attribution List from the producer. The Consumer then receives the list once it is available.
Note: The requests and responses are not real-time as the Producer may have to perform work to prepare and make the list available. The initial version of the implementation guide will focus on this specific exchange pattern.
Pattern 3: In pattern 3, the Producer notifies the Consumer of changes in the Member Attribution List. The Consumer requests for the changes and eventually receives incremental changes.
Note: The requests and responses are not real-time as the Producer may have to perform work to prepare and make the list available. Future versions of the implementation guide will focus on this specific exchange pattern.
Pattern 4: In pattern 4, the Consumer requests changes to the Member Attribution List and then the rest of the interactions follow exchange pattern #3.
Note: Future versions of the implementation guide will focus on this specific exchange pattern.
Pattern 5: In pattern 5, the Consumer provides an initial attribution list to the Producer. This could be based on the patients being treated by the provider. This is true in Data at Point of Care use cases. The rest of the interactions follow exchange pattern #3.
Note: Future versions of the implementation guide may focus on this specific exchange pattern depending on the extent it applies to the commercial payer and provider ecosystem.
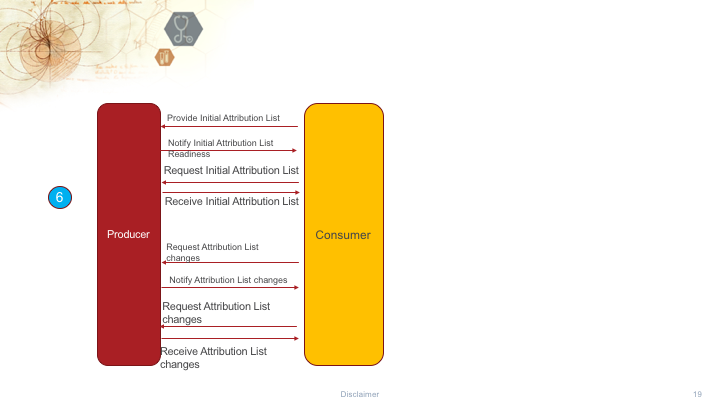
Pattern 6: In pattern 6, the interactions are essentially combination of patterns #5, #4, #3 and #2.