This page is part of the US Core (v6.0.0: STU6) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 8.0.1. For a full list of available versions, see the Directory of published versions. Page versions: R7 R6
The US Core FHIR Profiles are designed to be the base set of requirements for FHIR implementation in the US. All US Realm implementation guides SHALL use the US Core Profiles or SHALL explicitly state why they are unable to use. Throughout the development of US Core, implementers, the government, and the clinical community have brought forward additional requirements for US Core. This section outlines the approach to growth and a place for items that may be added to US Core.
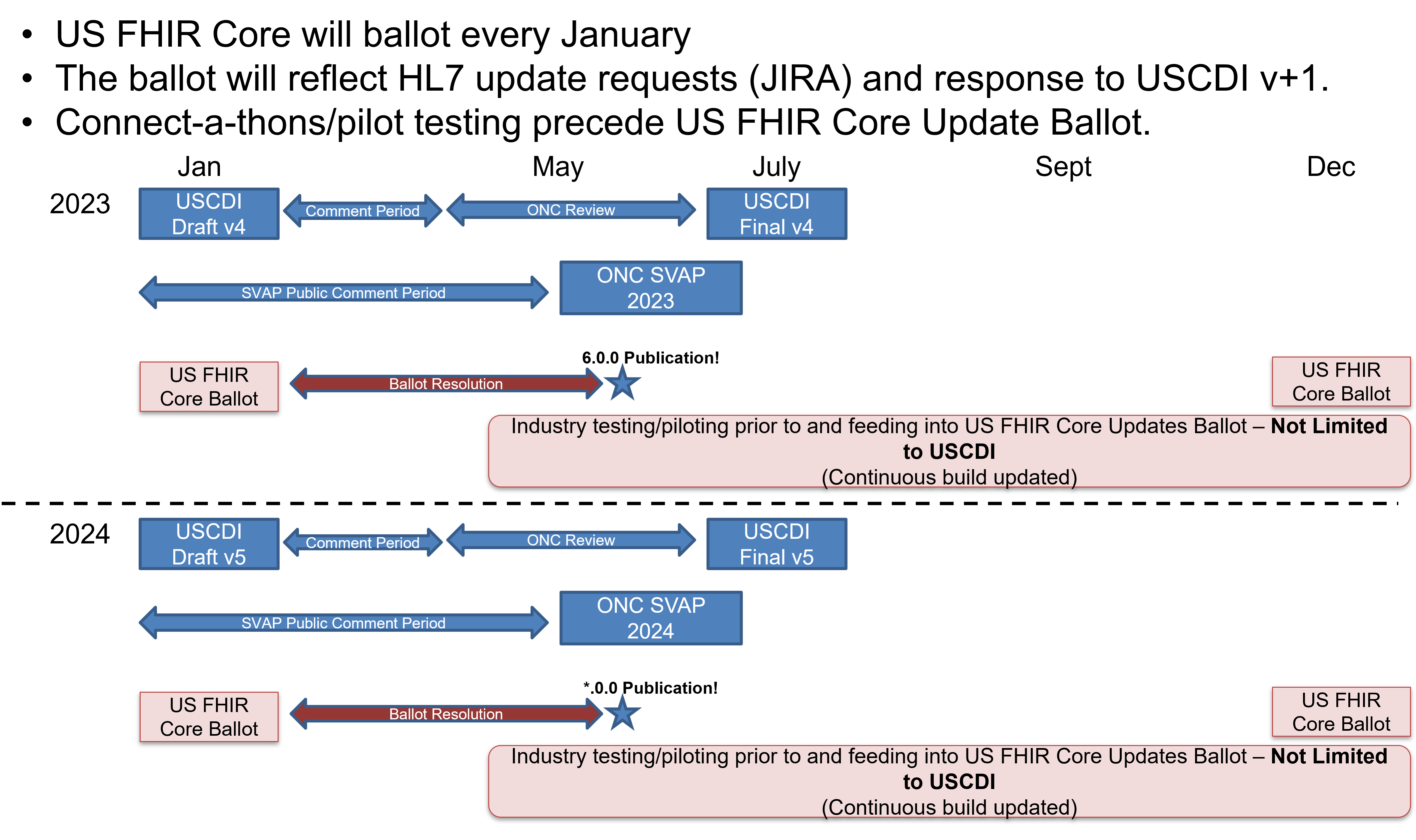
Yearly US Core updates reflect changes to U.S. Core Data for Interoperability (USCDI) and requests from the US Realm FHIR community. This approach is outlined in the figure below:
The US Core implementation Guide will grow following these steps:
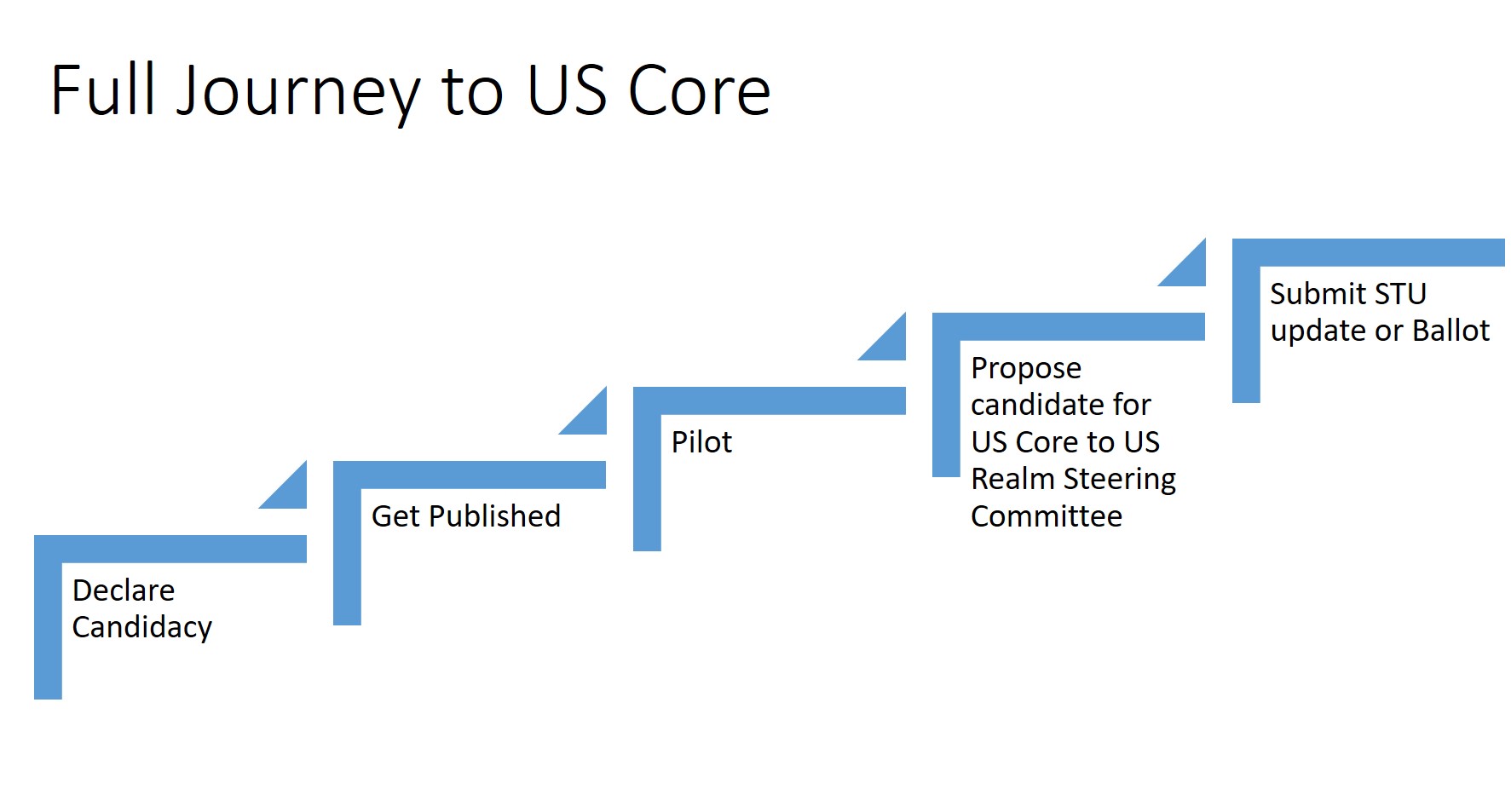
A new US Regulatory requirement may jump over some of these steps. However, regulators SHOULD be encouraged to complete pilot testing. With pilot testing, it is easier to understand how a change will affect real-world implementation.
Past Balloters, STU commenters, and Accelerator Project teams submitted the following items for consideration to add US Core. Additional requirements gathering is required before testing may occur on these items:
In the January ballot of 2019 we tested this process with the FDA requesting US Core include all the parts of UDI. In prior efforts, the FDA had successfully enhanced the base FHIR specification to include the UDI components.
The US Core Implantable Device Profile is intended to only be used for implantable devices. Please submit your successful implementation of a general non-implantable Device Profile (for example, software or crutches) for consideration in a future update of US Core.
The US Core design is based on the assumption that access to the Active Medication List is through searching MedicationRequest. (See: https://build.fhir.org/ig/HL7/US-Core/medication-list-guidance.html) The orders (MedicationRequest) capture all the medications, whether they have been fulfilled. MedicationAdministration can be used as well, but systems will need to be careful to link to appropriate MedicationRequest. Future versions of US Core may test and add MedicationAdministration.
Searching for multiple patients has been called out in the ONC Health IT Certification Program. Defining capabilities for multiple patient access would focus on querying real-time data for a user-facing provider app across patients. Examples of the type of queries that would be addressed include searching for all of a provider’s patients:
Clients currently face challenges displaying the source data’s times and timezone regardless of the end user’s current timezone. A solution is to define requirements and best practices for servers to preserve and represent time offsets and time zones.
A timezone is a geographical region in which residents observe the same standard time. A time offset is an amount of time subtracted from or added to Coordinated Universal Time (UTC) time to get the current civil time, whether it is standard time or daylight saving time (DST).1
Common practice is to preserve the source data time offsets as the original offset or converted to Coordinated Universal Time (UTC) time. Making this a requirement is one consideration. Another consideration is the addition of server best practices for preserving source timezones using the FHIR standard timezone extension. A third consideration is providing a client algorithm for resolving time offsets and time zones.
Very little guidance is provided on writing and updating data in the context of US Core Profiles. There are multiple issues that will need to be considered when defining expected behavior by the various actors to support updates and writes to the data, including:
Because of FHIR’s resource-based data model, related but distinct data tend to be grouped together in the same FHIR resource type. The original SMART on FHIR scope syntax (and US regulation) tends to limit authorization servers to granting access to all data in the same FHIR resource type, or not giving access to all. For example, a patient can only share an encounter diagnosis if they share their entire problem list, or a health system can only enable backend access to a patient cohort’s SDOH data if it enables access to labs.
Since version 2.0.0 of SMART App Launch clients and servers have more specific control over shared data within a specific resource type using granular scopes. US core encourages user experimentation with granular scope and is seeking general feedback. In addition, specific feedback is sought on best practices around scope string length and JWT-based tokens.
SMART on FHIR STU2 introduced a scope syntax of: <patient|user|system> / <fhir-resource>. <c | r | u | d |s> [?param=value]
For example, to limit read and search access to a specific patient’s laboratory observations but not other observations, the server grants the following scope:
patient/Observation.rs?category=http://terminology.hl7.org/CodeSystem/observation-category|laboratory.
We propose to use only a portion of the full expressivity of the FHIR search syntax by limiting initial scopes to:
The example scopes below use a single FHIR search parameter of category applied to Condition and Observation. They use a system/ prefix, but implementers can also support patient/ and user/.
system/Condition.rs?category=http://terminology.hl7.org/CodeSystem/condition-category|encounter-diagnosissystem/Condition.rs?category=http://terminology.hl7.org/CodeSystem/condition-category|problem-list-itemsystem/Condition.rs?category=http://hl7.org/fhir/us/core/CodeSystem/condition-category|health-concernsystem/Observation.rs?category=http://terminology.hl7.org/CodeSystem/observation-category|clinical-testsystem/Observation.rs?category=http://terminology.hl7.org/CodeSystem/observation-category|laboratorySee the respective “Quick Start” section on each US Core Profile page for more examples.
Footnotes
https://en.wikipedia.org/w/index.php?title=UTC_offset#Time_zones_and_time_offsets ↩