This page is part of the CodeX™ Radiation Therapy (v1.0.0-ballot: STU 1 Ballot 1) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.0.0. For a full list of available versions, see the Directory of published versions
Radiation therapy treatment details – critical for care coordination – are not readily available in information systems beyond radiation oncology information technology (IT) modules. Furthermore, creation of radiation therapy (RT) treatment summary documents is often a manual process, creating clinician burden and potential patient safety issues. Historical RT summary documents tend to be comprised of unstructured data; therefore, providers have been unable to leverage this information to meet reporting requirements (e.g., quality reporting, registry reporting) or support comparative effectiveness research without additional manual data entry.
This lack of cohesion, coordination, and structured data sharing between Radiation Oncology Information Systems (ROIS) and other health information systems is due to the lack of standardized data in the radiation oncology domain and absence of Fast Healthcare Interoperability Resources (FHIR) standards to support data transmission. Radiation oncology is highly specialized. A clinically relevant and accurate treatment summary is needed by both the larger oncology care team to facilitate care coordination, and by patients to better understand the care they have received. There is a demonstrated need to establish data standardization for RT end-of-treatment summaries, in-progress summaries, and supporting clinical details to supplement these summary reports. The CodeX Radiation Therapy Implementation Guide (IG) describes how to represent, model, and exchange RT information that is generated during a patient’s RT planning and treatment. This FHIR IG is intended for health information system implementers interested in sending or receiving RT information. The CodeX RT IG provides nine profiles based on FHIR ServiceRequest and Procedure resources, and one based on the FHIR BodyStructure resource. These profiles support radiotherapy clinical workflow by:
Once structured data is captured during the care process, that data can be made available for data sharing and reuse. The CodeX RT IG leverages FHIR and FHIR Application Programming Interfaces (APIs) to promote interoperable exchange of RT information between an ROIS and other health information systems such as an electronic health record (EHR). The CodeX RT IG has defined radiotherapy FHIR profiles for vendors to implement in their systems and share, via FHIR API, with other FHIR-enabled radiation oncology information systems or EHRs.
The Codex RT IG builds on the minimal Common Oncology Data Elements (mCODE) Standard for Trial Use 2 (STU 2), leveraging mCODE’s Radiotherapy Course Summary and Radiotherapy Volume resource profiles, and associated value sets and extensions. The mCODE STU 2 IG also includes a Radiotherapy Glossary that contains all key terms, their definitions, and related examples. The remaining radiotherapy concepts are defined in this IG.
The intended actors include:
The intended use cases include:
A radiation oncologist generates a patient’s RT “end-of-treatment” summary within the ROIS after treatment is complete. The patient’s summary information is pushed, via a FHIR API, to a receiving FHIR repository (e.g., a cloud-based repository or another repository that can be accessed by other vendors). Next, a vendor system accesses the FHIR repository via a FHIR API call to retrieve the patient’s RT “end-of-treatment” information. Once the information has been retrieved, the vendor system can store, share, reuse, and display the standardized information however necessary/most useful.
A radiation oncologist generates a patient’s weekly on-treatment visit (OTV) report within the ROIS. The patient’s weekly RT in-progress information is pushed, via a FHIR API, to an EHR’s FHIR-enabled internal resource repository. Next, the EHR accesses its internal FHIR repository via a FHIR API call and retrieves the patient’s weekly RT in-progress information. Once the information has been retrieved, the EHR can store, share, reuse, and display the standardized information however necessary/most useful.
The profiles defined in this IG cover different stages of the radiotherapy workflow at different levels of detail. A radiotherapy course systematically addresses a condition or set of related conditions. The course can include multiple sessions, can be divided into multiple phases, and can last for several months. The Radiotherapy Course Summary profile covers the treatment delivered in a treatment course and can be incrementally updated as the treatment progresses. When the treatment is completed, the latest version of the Radiotherapy Course Summary provides the entire course of treatment from beginning to end. The status element indicates whether the treatment is in progress or complete.
In radiotherapy, a phase is a subset of a course. A phase is defined as a treatment consisting of one or more identical fractions. See the Radiotherapy Glossary.
At the most detailed level, treatment plans define how the radiotherapy treatment is delivered.
Note that in radiotherapy, a treatment plan represents a concrete set of treatment delivery instructions prepared for a specific patient anatomy and machine (Radiotherapy Glossary). It is the most specific and most detailed concept in this model. The concept of a radiotherapy treatment plan includes the lowest level of machine instructions to control a treatment device. However, these details are not modelled in the FHIR representation of a radiotherapy treatment plan. Instead, the respective ServiceRequest (Radiotherapy Treatment Plan) includes an extension to reference the DICOM artifacts that define the machine geometry and motion during treatment. The Procedure that records the delivered treatment (Radiotherapy Treated Plan), references DICOM treatment records that contain all machine details.
The relationship between a course, phases, and treatment plans is exemplified in the following diagram.
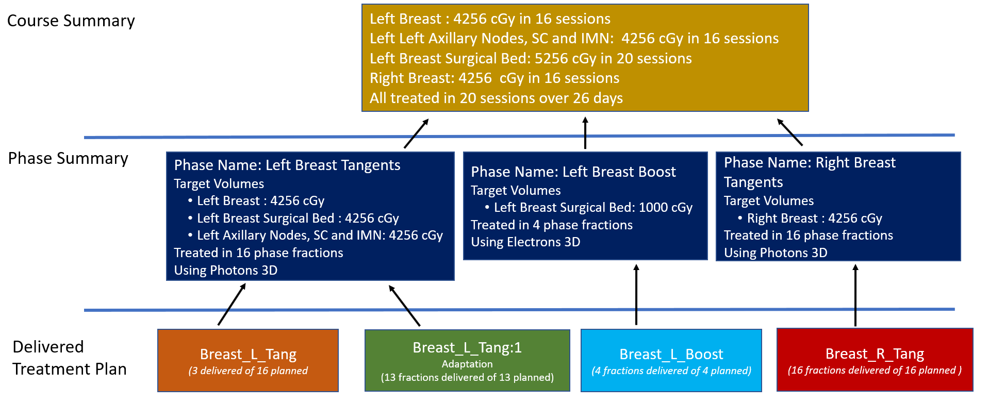
In this example, the radiotherapy course encompasses three phases. The course summary captures each radiotherapy volume, the total dose for each volume, and total number of fractions delivered for each volume. The course summary also records the modalities and techniques used, without directly associating those with individual volumes. Other elements in the summary include the reason for treatment, the treatment intent, the period of treatment, and the total number of sessions.
At the phase level, each phase consists of a set of identical fractions. In this context, identical means that each fraction uses the same modality, technique, dose per fraction, and is applied to the same volume or volumes. Because of their spatial relationship or the technique used, all volumes do not necessarily receive the same total dose during a phase. Phases may occur in parallel, overlap, or in alternating temporal patterns.
Multiple treatment plans may be used to implement the same phase. Plans may be adapted during a phase due to changes in tumor shape, patient anatomy, or side effects. In the extreme case of adaptive treatment with daily adaptation, a new plan may be created for each fraction of a phase.
The following figure shows the resource profiles to represent the radiotherapy requests and procedures at different levels. Note that the radiotherapy prescriptions and plans are instances of patient specific requests, not templates or protocols. They are therefore modelled as ServiceRequest. These requests may be embedded in a higher level CarePlan, which coordinates various activities of the radiotherapy workflow, but radiotherapy CarePlans are not scope of this IG.
While treatment is in progress, a consumer of these resources can retrieve the current version of the in-progress Radiotherapy Course Summary to get the current state of treatment delivery. If interested in how the treatment is structured, the observer can also retrieve the lower-level Procedures. A treatment observer can additionally retrieve the ServiceRequests referenced from these Procedures to find what was planned and prescribed. A typical overview of how far the treatment has progressed can be created by comparing the delivered dose and number of fractions in the Treated Phases to the respective planned dose and number of fractions in the Planned Phases.
The diagram below shows the relationship between the RT profiles and data elements. It also highlights which are extensions developed as part of the RT FHIR data model.
The workflow and transactions for exchanging RT information are documented in the Integrating Healthcare Enterprise - Radiation Oncology (IHE-RO) Exchange of Radiotherapy Summaries (XRTS) Supplement. These XRTS transactions utilize the FHIR profiles defined in the CodeX RT IG.
In late 2020, the American Society for Radiation Oncology (ASTRO) and the American Association of Physicists in Medicine (AAPM), with the assistance of the MITRE Corporation, proposed a use case under the CodeX FHIR Accelerator around standardizing RT information using the FHIR standard to semantically define a patient’s radiation therapy end-of-treatment information. This group of stakeholder organizations began working on defining RT concepts, leveraging mCODE and FHIR, to model the relationship between groups of clinical concepts that comprise work products vital to radiation oncology care.
In January 2021, the CodeX Radiation Therapy Treatment Data (RTTD) project approached the Integrating the Healthcare Enterprise – Radiation Oncology (IHE-RO) Exchange of Radiotherapy Summaries (XRTS) Work Group about aligning the data model and FHIR structures with the technical architecture and transactions being defined in the XRTS technical specification document. The CodeX RTTD and XRTS teams aligned visions and began working together to adopt the CodeX RT Implementation Guide.
In support of this collaboration, radiotherapy profiles were added to mCODE STU2, Radiotherapy Course Summary and Radiotherapy Volume, as well as other value sets and extensions required to represent a radiotherapy treatment summary.
Radiotherapy specifications beyond what was considered “minimal” (which is a tenet of mCODE) are published in this CodeX RT IG.
Furthermore, the radiotherapy profiles and data elements were tested in IHE-RO XRTS Workshops December 2021 and May 2022. The CodeX RTTD and IHE-RO XRTS teams will continue to test the CodeX RT IG at future IHE-RO XRTS Workshops and Connectathons.
Additional details regarding the CodeX RTTD project:
Specifications in the CodeX RT IG were informed by research and work products developed by the AAPM Big Data Subcommittee (BDSC). AAPM BDSC has been using a consensus-driven approach to define a common ontology that will improve communication of RT information. The standardized nomenclatures created by the BDSC team are represented in OORO. BDSC participants include AAPM, ASTRO, Canadian Organization of Medical Physicists (COMP), European Society for Radiotherapy and Oncology (ESTRO), NRG Oncology, Canadian Association of Radiation Oncology (CARO), IHE-RO, and Canadian Partnership for Quality Radiotherapy (CPQR).
In addition to information obtained from subject matter experts, several existing standards, nomenclatures, and guidelines were consulted during the development of this specification. These include:
In addition, material was drawn from the US Core Implementation Guide and the mCODE Implementation Guide.
“Building” the IG means generating a web-based, human-readable representation of the structured information and accompanying documentation defined within this repository. This is done via the FHIR Implementation Guide Publisher (“IG Publisher”), a Java program provided by the FHIR team for building IGs into a standardized presentation.
If you would like to generate this locally, open command prompt window and navigate to the directory where this repository has been cloned. Then run this command:
./_genonce.sh_genonceThis script will do two things automatically for you:
Run SUSHI. This IG is developed developed in FHIR Shorthand (FSH), a domain-specific language (DSL) for defining the content of FHIR IGs. SUSHI complies FSH files into the JSON files expected by the IG Publisher.
Run the IG Publisher.
You will need an active internet connection to build the IG. It make take up to 30 minutes to build for the first time; subsequent builds should be faster (5-7 minutes) on a modern laptop.
When the build finishes, you can open output/index.html in your browser to see the locally built IG.
./_updatePublisher.sh (Linux/macOS) or _updatePublisher.bat (Windows) to download the IG Publisher.If you want to run SUSHI without building the entire IG, you can run sushi . in a command prompt window after navigating to the directory where this repository has been cloned.
You can also run the IG Publisher without running SUSHI with ./_genonce.sh -no-sushi or _genonce -no-sushi.
While not normally necessary, you can delete the following folders to get a clean build:
fsh-generated/ (SUSHI output)output/ (IG Publisher output)input-cache/ (IG Publisher local cache; note that deleting this will dramatically increase the length of the next build).fsh) files defining the resources in this IG are found in input/fsh/.
The FSH files are prefixed based on what is contained inside.
| Prefix | Description |
|---|---|
AL |
Aliases |
DEF |
Other Definitions |
EX |
Examples |
SD |
StructureDefinitions |
VS |
ValueSets |
input/pagecontent/. These pages must also be included in sushi-config.yaml to be compiled to HTML by the IG Publisher.sushi-config.yaml including the menu contents of the built IG and the groupings on the Artifacts Summary page.The authors gratefully acknowledge the contributions of Chuck Mayo, PhD, University of Michigan/AAPM, Randi Kudner, MFA, ASTRO, John Kildea, PhD, McGill University/COMP, Mary Feng, MD, University of California San Francisco/ASTRO, James Hayman, MD, University of Michigan/ASTRO, Rishabh Kapoor, PhD, Virginia Commonwealth University/AAPM, John Christodouleas, MD, University of Pennsylvania/Elekta, Michelle Casagni, MS, MITRE, Su Chen, MD, MITRE, Anthony DiDonato, MS, MITRE, Sharon Sebastian, RN-BC, MS, MITRE.
The authors recognize HL7 sponsorship and input from Cross-Group Projects.
Steve Bratt leads the CodeX FHIR Accelerator, a member-driven community with a core goal of leveraging FHIR-based standards to achieve interoperability within the healthcare community to improve health for all.
Many organizations have been involved in the modeling and defining of the radiotherapy FHIR profiles that are defined in the CodeX RT IG:
The RTTD team also receives significant input and participation from:
If you have questions or comments about this guide, you can join the conversation on the CodeX Radiation Therapy stream on zulip, create an issue in the HL7 Jira, or reach out to any of the following individuals:
| Topic | Who | Role | |
|---|---|---|---|
| Implementation and Use Cases | Steve Bratt | CodeX Accelerator Program Manager | sbratt@mitre.org |
| Topic | Martin Von Siebenthal (Varian, a Siemens Healhtineers Company) | Primary Author | martin.vonsiebenthal@varian.com |
| Topic | Saul A. Kravitz (MITRE) | Author | saul@mitre.org |
CodeX Radiation Therapy is an open source project and welcomes all contributors. The source code for this IG is maintained in the HL7 Github. All of the profiling work is done using FHIR Shorthand and SUSHI.