This page is part of the Consumer Real-time Pharmacy Benefit Check (v1.0.0: STU 1) based on FHIR R4. This is the current published version. For a full list of available versions, see the Directory of published versions 
Format(s):
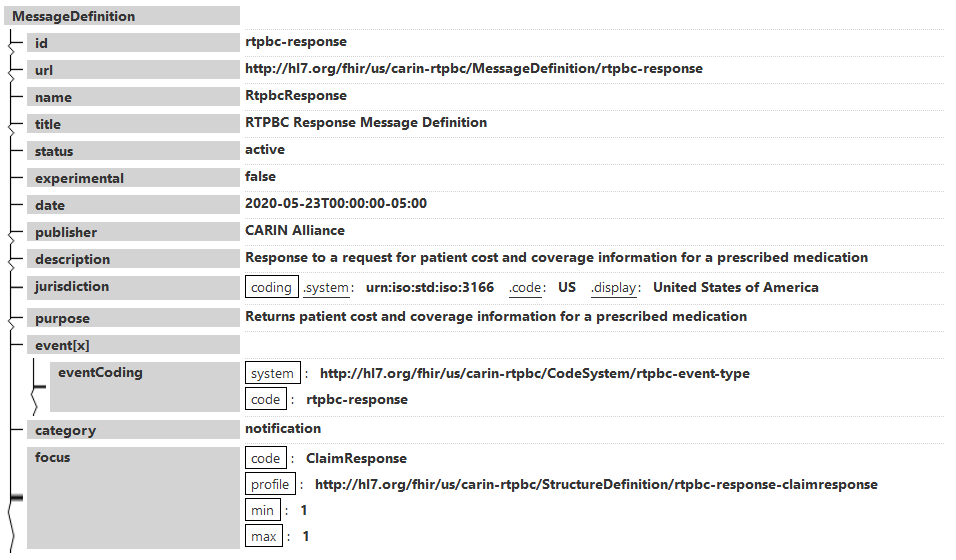
This MessageDefinition describes the content of a real-time pharmacy benefit check (RTPBC) response, when using FHIR messaging.
The ClaimResponse resource returns patient pricing and coverage information upon successful processing at the RTPBC source. (An OperationOutcome is returned when an error is encountered)
Note: The guide describes two methods for submitting the RTPBC request ($submit operation and FHIR messaging using $process-message), with the intent to elicit comments from potential implementers.
Narrative view
Generated Narrative
id: rtpbc-response
url: http://hl7.org/fhir/us/carin-rtpbc/MessageDefinition/rtpbc-response
version: 1.0.0
name: RtpbcResponse
title: RTPBC Response Message Definition
status: active
experimental: false
date: May 23, 2020 5:00:00 AM
publisher: HL7 International - Pharmacy
contact: HL7 International - Pharmacy: http://www.hl7.org/Special/committees/medication, Frank McKinney: frank.mckinney@pocp.com
description: Response to a request for patient cost and coverage information for a prescribed medication
jurisdiction: United States of America
purpose: Returns patient cost and coverage information for a prescribed medication
event: RTPBC Response
category: notification
| - | Code | Profile | Min | Max |
| * | ClaimResponse | http://hl7.org/fhir/us/carin-rtpbc/StructureDefinition/rtpbc-response-claimresponse | 1 | 1 |