This page is part of the Consumer Real-time Pharmacy Benefit Check (v1.0.0: STU 1) based on FHIR R4. This is the current published version. For a full list of available versions, see the Directory of published versions 
Format(s):
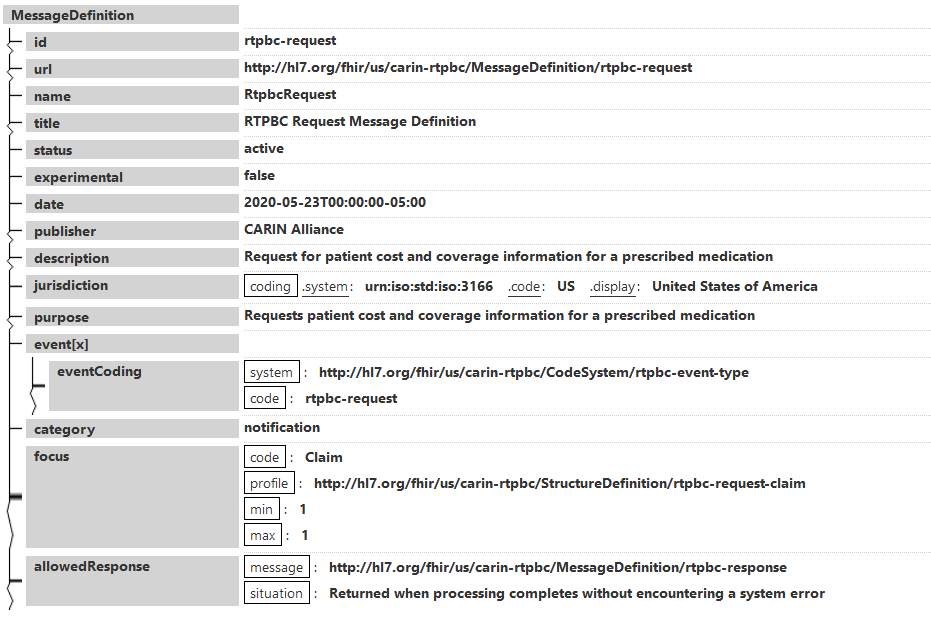
This MessageDefinition describes the content of a real-time pharmacy benefit check (RTPBC) request, when using FHIR messaging.
The Claim resource is the focus in a bundle that also contains other supporting resources referenced by the Claim (Patient, MedicationRequest, Coverage, Practitioner, Organization).
Note: The guide describes two methods for submitting the RTPBC request ($submit operation and FHIR messaging using $process-message), with the intent to elicit comments from potential implementers.
Narrative view
Generated Narrative
id: rtpbc-request
url: http://hl7.org/fhir/us/carin-rtpbc/MessageDefinition/rtpbc-request
version: 1.0.0
name: RtpbcRequest
title: RTPBC Request Message Definition
status: active
experimental: false
date: May 23, 2020 5:00:00 AM
publisher: HL7 International - Pharmacy
contact: HL7 International - Pharmacy: http://www.hl7.org/Special/committees/medication, Frank McKinney: frank.mckinney@pocp.com
description: Request for patient cost and coverage information for a prescribed medication
jurisdiction: United States of America
purpose: Requests patient cost and coverage information for a prescribed medication
event: RTPBC Request
category: notification
| - | Code | Profile | Min | Max |
| * | Claim | http://hl7.org/fhir/us/carin-rtpbc/StructureDefinition/rtpbc-request-claim | 1 | 1 |
| - | Message | Situation |
| * | http://hl7.org/fhir/us/carin-rtpbc/MessageDefinition/rtpbc-response | Returned when processing completes without encountering a system error |