This page is part of the Consumer Real-time Pharmacy Benefit Check (v1.0.0: STU 1) based on FHIR R4. This is the current published version. For a full list of available versions, see the Directory of published versions 
Format(s):
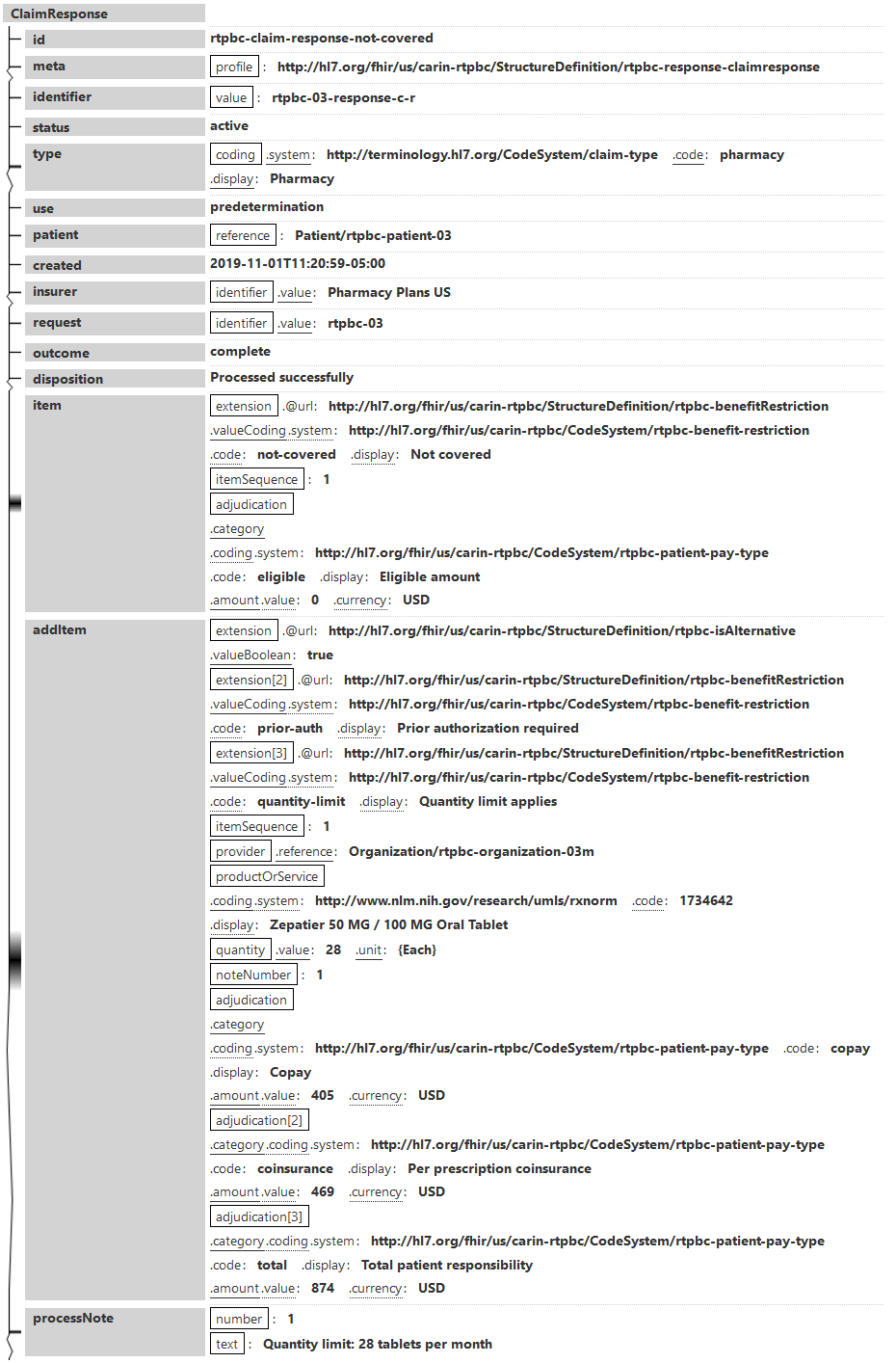
In this example:
Narrative view
Generated Narrative
id: rtpbc-claim-response-not-covered
meta:
identifier: id: rtpbc-03-response-c-r
status: active
type: Pharmacy
use: predetermination
created: Nov 1, 2019 4:20:59 PM
insurer:
request:
outcome: complete
disposition: Processed successfully
item
itemSequence: 1
Adjudications
- Category Amount * Eligible amount
addItem
itemSequence: 1
productOrService: Zepatier 50 MG / 100 MG Oral Tablet
quantity: 28 {Each}
noteNumber: 1
Adjudications
- Category Amount * Copay * Per prescription coinsurance * Total patient responsibility
| - | Number | Text |
| * | 1 | Quantity limit: 28 tablets per month |