This page is part of the FHIR Specification (v5.0.0-ballot: FHIR R5 Ballot Preview). The current version which supercedes this version is 5.0.0. For a full list of available versions, see the Directory of published versions  . Page versions: R5 R4B R4 R3 R2
. Page versions: R5 R4B R4 R3 R2
Security  Work Group Work Group | Maturity Level: 4 | Standards Status: Trial Use |
Fast Healthcare Interoperability Resources (FHIR) is not a security protocol, nor does it define any security related functionality. However, FHIR does define exchange protocols and content models that need to be used with various security protocols defined elsewhere. This section gathers all information about security in one section. A summary:
 where appropriate.
where appropriate.
Time critical concerns regarding security flaws in the FHIR specification should be addressed to
the FHIR email
list  for prompt consideration.
for prompt consideration.
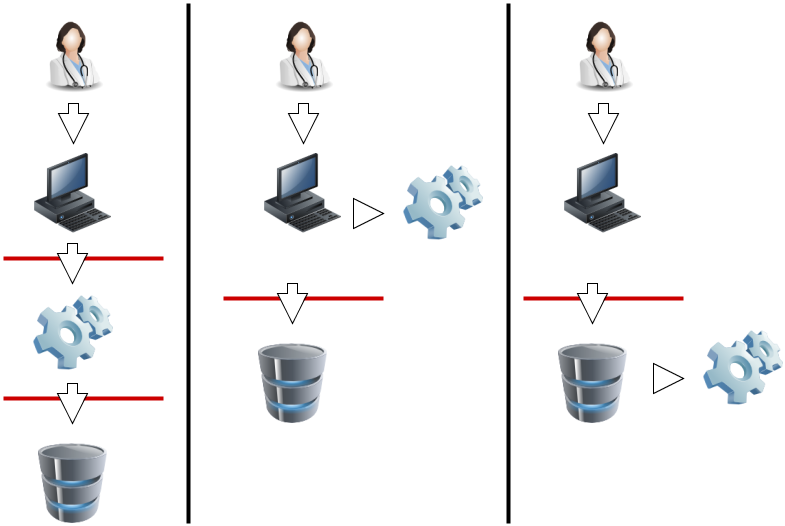
A production FHIR system will need some kind of security sub-system that administers users, user authentication, and user authorization. Where this subsystem fits into the deployment architecture is a matter for system design:
|
|
In this diagram, the red lines represent FHIR interfaces. From the perspective of the FHIR API, the client (consumer of FHIR services) may either interact with a security system that manifests as a FHIR server, and which depends on a subsequent FHIR interface to provide the actual storage, or either the client or server interacts with the security system independently. In each of these 3 scenarios, the different components may be assembled into applications or network components differently, but the same logical layout applies. The FHIR specification assumes that a security system exists, and that it may be deployed in front of or behind the FHIR API.
The security system includes the following subsystems:
Because there are a plethora of standards relating to the administration and functionality of the security system, FHIR does not provide user, profile, or other such administration resources. Instead, the FHIR resources are the targets of the policies expressed in these other approaches. What FHIR does specify is a way to apply security labels to resources so that a security system may use these (along with the contents of the resources if appropriate) to determine whether a user is authorized to perform a particular FHIR operation or not.
The appropriate protections for Privacy and Security are specific to the risks to Privacy and the risks to Security of that data being protected. This concept of appropriate protections is a very specific thing to the actual data. Any declaration of 'required' or 'optional' requirements that could be mentioned here are only recommendations for that kind of Resource in general for the most common use of that Resource. Where one uses the Resource in a way that is different than this most common use, one will have different risks and thus need different protections. Each Resource is indicated with the common "Security Category", and all of the Resources Security Category is shown on the Resource Types page with the Security Category tab.
Most Resources will need some form of Access Control to Create, Update, or Delete. The following general guidance is given only as general guidance for READ and QUERY access:
These resources tend to not contain any individual data, or business sensitive data. Most often these Resources will be available for anonymous access, meaning there is no access control based on the user or system requesting. However, these Resources do tend to contain important information that must be authenticated back to the source publishing them, and protected from integrity failures in communication. For this reason, server authenticated https (TLS) is recommended to provide authentication of the server and integrity protection in transit. This is normal web-server use of https.
These Resources tend to not contain any individual data, but do have data that describe business or service sensitive data. The use of the term Business is not intended to only mean an incorporated business, but rather the broader concept of an organization, location, or other group that is not identifiable as individuals. Often these resources will require some sort of client authentication to assure that only authorized access is given. The client access control may be to individuals, or may be to system identity. For this purpose, possible client authentication methods such as: mutual-authenticated-TLS, APIKey, App signed JWT, or App OAuth client-id JWT For example: an App that uses a Business protected Provider Directory to determine other business endpoint details.
These Resources do NOT contain Patient data, but do contain individual information about other participants. These other individuals are Practitioners and PractitionerRole. These identities are needed to enable the practice of healthcare. These identities are identities under general privacy regulations, and thus must consider Privacy risk. Often access to these other identities are covered by business relationships. For this purpose, access to these Resources will tend to be Role specific using methods such as RBAC or ABAC.
These Resources make up the bulk of FHIR and therefore are the most commonly understood. These Resources contain highly sensitive health information, or are closely linked to highly sensitive health information. These Resources will often use the security labels to differentiate various confidentiality levels within this broad group of Patient Sensitive data. Access to these Resources often requires a declared Purpose Of Use. Access to these Resources is often controlled by a Privacy Consent. See the section below on Authorization and Access Control.
Some Resources can be used for a wide scope of use-cases that span very sensitive to very non-sensitive. These Resources do not fall into any of the above classifications, as their sensitivity is highly variable. These Resources will need special handling. These Resources often contain metadata that describes the content in a way that can be used for Access Control decisions.
For the RESTful API, normal HTTP security rules apply.
Please follow the HTTP specification Security Considerations section 9  .
The Service Base URL will specify whether TLS is required.
Client authentication may be required by the server, possibly including the requirement for
client certificates.
When returning responses to non-authorized clients, ensure that Hypertext Transfer Protocol (HTTP) headers of a web server and API error messages or faults do not disclose detailed information about the underlying web server that could be the source of potential exploitation.
.
The Service Base URL will specify whether TLS is required.
Client authentication may be required by the server, possibly including the requirement for
client certificates.
When returning responses to non-authorized clients, ensure that Hypertext Transfer Protocol (HTTP) headers of a web server and API error messages or faults do not disclose detailed information about the underlying web server that could be the source of potential exploitation.
Please follow IETF Best Current Practice (BCP 195  ) - "Recommendations for Secure Use of Transport Layer Security (TLS) and Datagram Layer Security (DTLS)"
) - "Recommendations for Secure Use of Transport Layer Security (TLS) and Datagram Layer Security (DTLS)"  .
.
Consider using additional methods of security for an API to help authenticate where Domain Name System (DNS) responses are coming from and ensure that they are valid. For example, the use of Domain Name System Security Extensions (DNSSEC), a suite of extensions that add security to the DNS protocol, can ensure that domains associated with API endpoints that transmit health information or information required for API access are secure. DNSSEC provides origin authority, data integrity, and authenticated denial of existence. With DNSSEC, the DNS protocol is much less susceptible to certain types of attacks, particularly DNS spoofing attacks.
The TLS communications are established prior to any HTTP command/response, so the whole FHIR interaction is protected by the TLS communications. The security of the endpoints of the TLS communications must be risk-managed, so as to prevent inappropriate risks (e.g. audit logging of the GET parameters into an unprotected audit log).
When it is desirable to support browser-based javascript client applications, servers SHOULD consider
enabling cross-origin resource sharing (CORS)  for the REST operations.
Consider advice from sources including Enable-CORS
for the REST operations.
Consider advice from sources including Enable-CORS  and Moesif blog on Guide to CORS Pitfalls
and Moesif blog on Guide to CORS Pitfalls  .
Experience shows that this is an area where ongoing issues may be expected as security holes are found and closed on an ongoing basis.
.
Experience shows that this is an area where ongoing issues may be expected as security holes are found and closed on an ongoing basis.
Other than testing systems, FHIR servers should authenticate the clients.
The server may choose to authenticate the client system and trust it, or to authenticate
the individual user by a variety of techniques. For web-centric environments it is recommended to use
OpenID Connect  (or other suitable authentication protocol) to verify identity of the end user, where it is necessary that end-users be identified to the application.
(or other suitable authentication protocol) to verify identity of the end user, where it is necessary that end-users be identified to the application.
All systems shall protect authenticator mechanisms, and select the type of credential/strength of authenticator based on use-case and risk management.
Correctly identifying people, devices, locations and organizations is one of the foundations that any security system is built on. Most applications of security protocols, whether authentication, access control, digital signatures, etc. rely on the correct mapping between the relevant resources and the underlying systems. Note that this isn't necessary. There is nothing in FHIR that requires or relies on any security being in place, or any particular security implementation. However, real world usage will generally require this.
A holder of data should not allow the data to be communicated unless there are enough assurances that the other party is authorized to receive it. This is true for a client creating a resource through a PUT/POST, as much as it is true for a server returning resources on a GET. The presumption is that without proper authorization, to the satisfaction of the data holder, the data does not get communicated.
Two of the classic Access Control models are: Role-Based Access Control (RBAC), and Attribute-Based Access Control (ABAC).
In Role-Based Access Control (RBAC), permissions are operations on an object that a user wishes to access. Permissions are grouped into roles. A role characterizes the functions a user can perform. Roles are assigned to users. If the user's role has the appropriate permissions to access an object, then that user is granted access to the object. FHIR readily enables RBAC, as FHIR Resources are object types and the CRUDE (Create, Read, Update, Delete, Execute) events (the FHIR equivalent to permissions in the RBAC scheme) are operations on those objects.
In Attribute-Based Access Control (ABAC), a user requests to perform operations on objects. That user's access request is granted or denied based on a set of access control policies that are specified in terms of attributes and conditions. FHIR readily enables ABAC, as instances of a Resource in FHIR (again, Resources are object types) can have attributes associated with them. These attributes include security tags, environment conditions, and a host of user and object characteristics, which are the same attributes as those used in ABAC. Attributes help define the access control policies that determine the operations a user may perform on a Resource (in FHIR) or object (in ABAC). For example, a tag (or attribute) may specify that the identified Resource (object) is not to be further disclosed without explicit consent from the patient.
The rules behind the access control decision are often very complex, and potentially depend on information sourced from:
For one source of further information, see the
IHE Access Control white paper 
Access control constraints may result in data returned in a read or search being redacted or otherwise restricted. See Variations between Submitted data and Retrieved data.
It is recommended that OAuth  be used to authenticate and/or authorize
the client and user. The HL7 SMART-On-FHIR
be used to authenticate and/or authorize
the client and user. The HL7 SMART-On-FHIR  Implementation Guide
on OAuth is a recommended method for using OAuth for authorizing interactions with a protected FHIR Server.
Implementation Guide
on OAuth is a recommended method for using OAuth for authorizing interactions with a protected FHIR Server.
The HEART Working Group  has developed a
set of privacy and security specifications that enable an individual to control the
authorization of access to RESTful health-related data sharing APIs, and to facilitate
the development of interoperable implementations of these specifications by others.
IHE IUA Profile
has developed a
set of privacy and security specifications that enable an individual to control the
authorization of access to RESTful health-related data sharing APIs, and to facilitate
the development of interoperable implementations of these specifications by others.
IHE IUA Profile  constrains OAuth token attributes to support Healthcare.
constrains OAuth token attributes to support Healthcare.
Another proposed model for managing and enforcing patient consents relies on an OAuth 2.0 server which uses the patient consents as the applicable authorization policies at the time of issuing a token. In this model, the authorization server (OAuth 2.0 or its User-Managed Access profile  ) examines the patient consent to determine whether or not to issue a token to a requesting client and what scopes to grant. The main motivation behind this model is to have a separate consent management system in charge of collecting, storing, and maintaining patient consents, as well as responding to authorization requests based on these consents. This facilitates having third-party consent management services to which organizations can outsource their consent management functions. Further details about this model are discussed in this report
) examines the patient consent to determine whether or not to issue a token to a requesting client and what scopes to grant. The main motivation behind this model is to have a separate consent management system in charge of collecting, storing, and maintaining patient consents, as well as responding to authorization requests based on these consents. This facilitates having third-party consent management services to which organizations can outsource their consent management functions. Further details about this model are discussed in this report  .
.
An extension to this model, Cascaded Authorization, enables an OAuth/UMA authorization server to require and rely on the approval of another OAuth/UMA server before issuing a token and granting scopes. Using this model, the enterprise OAuth/UMA server at a provider organization can rely on the decisions by a Consent OAuth/UMA Server by requiring and accepting access tokens issued by that server as part of the client authorization process. This architecture preserves the independence of a consent management system, which can potentially be outsourced to third-parties, while ensuring that all authorization interfaces and interactions follow the OAuth/UMA protocols. A summary of the concepts and flows for Cascaded Authorization are discussed in this report  . Further extensions to this model to leverage UMA’s capabilities to simplify some of the flows are discussed in this report
. Further extensions to this model to leverage UMA’s capabilities to simplify some of the flows are discussed in this report  . A reference implementation of Cascaded Authorization and more technical details can be found here
. A reference implementation of Cascaded Authorization and more technical details can be found here  .
.
Additionally, the Unified Data Access Profiles (UDAP)  propose extensions to the OAuth 2.0 framework to scale authorization; authentication; trusted Dynamic Client Registration; and Client Certification and Endorsements using JSON Web Tokens and X.509 certificates.
propose extensions to the OAuth 2.0 framework to scale authorization; authentication; trusted Dynamic Client Registration; and Client Certification and Endorsements using JSON Web Tokens and X.509 certificates.
A web-server, especially hosting FHIR, must choose the response carefully when an Access Denied condition exists. Returning too much information may expose details that should not be communicated. The Access Denied condition might be because of missing but required Authentication, the user is not authorized to access the endpoint, the user is not authorized to access specific data, or other policy reasons.
To balance usability of the returned result vs appropriate protection, the actual result method used needs to be controlled by policy and context. Typical methods of handling Access Denied used are:
Return a Success with Bundle containing zero results - This result is indistinguishable from the case where no data is known. When consistently returned on Access Denied, this will not expose which patients exist, or what data might be blinded. This method is also consistent with cases where some results are authorized while other results are blinded. This can only be used when returning a Bundle is a valid result.
Return a 404 "Not Found" - This also protects from data leakage as it is indistinguishable from a query against a resource that doesn't exist. It does however leak that the user authentication is validated.
Return a 403 "Forbidden" - This communicates that the reason for the failure is an Authorization failure. It should only be used when the client and/or user is well enough known to be given this information. Thus this method is most used when the user can know that they are forbidden access. It doesn't explain how the user might change things to become authorized.
Return a 401 "Unauthorized" - This communicates that user authentication was attempted and failed to be authenticated.
Note that if a server allows PUT to a new location, it is not feasible to return 404 Not Found. This means that clients can use this to test whether content exists that they are not able to access, which is a minor, but potentially significant, leak of information.
FHIR provides an AuditEvent resource suitable for use by FHIR clients and servers to record when a security or privacy relevant event has occurred. This form of audit logging records as much detail as reasonable at the time the event happened.
When used to record security and privacy relevant events, the AuditEvent can then be
used by properly authorized applications to support audit reporting, alerting, filtering,
and forwarding. This model has been developed and used in healthcare for a decade as
IHE-ATNA profile  .
ATNA log events can be automatically converted to AuditEvent resources, and from there,
client applications are able to search the audit events, or subscribe to them.
.
ATNA log events can be automatically converted to AuditEvent resources, and from there,
client applications are able to search the audit events, or subscribe to them.
For HTTP logs, implementers need to consider the implications of distributing access to the logs. HTTP logs, including those that only contain the URL itself, should be regarded as being as sensitive as the resources themselves. Even if direct PHI is kept out of the logs by careful avoidance of search parameters (e.g. by using POST), the logs will still contain a rich set of information about the clinical records.
Several FHIR resources include attachments. Attachments can either be references to content found elsewhere or included inline encoded in base64. Attachments represent security risks in a way that FHIR resources do not, since some attachments contain executable code. Implementers should always use caution when handling resources.
See Security Labels.
FHIR resources include an XHTML narrative, so that applications can display the contents of the resource to users
without having to fully and correctly process the data in the resource. However, displaying HTML is associated
with several known security issues that have been observed in production systems in other contexts (e.g.
with CDA  ). For
this reason, the FHIR narrative can't contain active content.
However, care is still needed when displaying the narrative:
). For
this reason, the FHIR narrative can't contain active content.
However, care is still needed when displaying the narrative:

Also note that the inclusion of an external reference to an image can allow the server that hosts the image to track when the resource is displayed. This may be a feature or a problem depending on the context.
In addition to narrative, Documents may also contain stylesheets. Unlike with CDA, the stylesheets are simple CSS stylesheets, not executable XSLT, so the same security risks do not apply. However, CSS stylesheets may still reference external content (e.g. background images), and applications displaying documents should ensure that CSS links are not automatically followed without checking their safety first, and that session/identifying information does not leak with any use of external links.