This page is part of the FHIR Specification (v1.8.0: STU 3 Draft). The current version which supercedes this version is 5.0.0. For a full list of available versions, see the Directory of published versions  . Page versions: R5 R4B R4 R3
. Page versions: R5 R4B R4 R3
Work Group Financial Management  | Ballot Status: n/a |
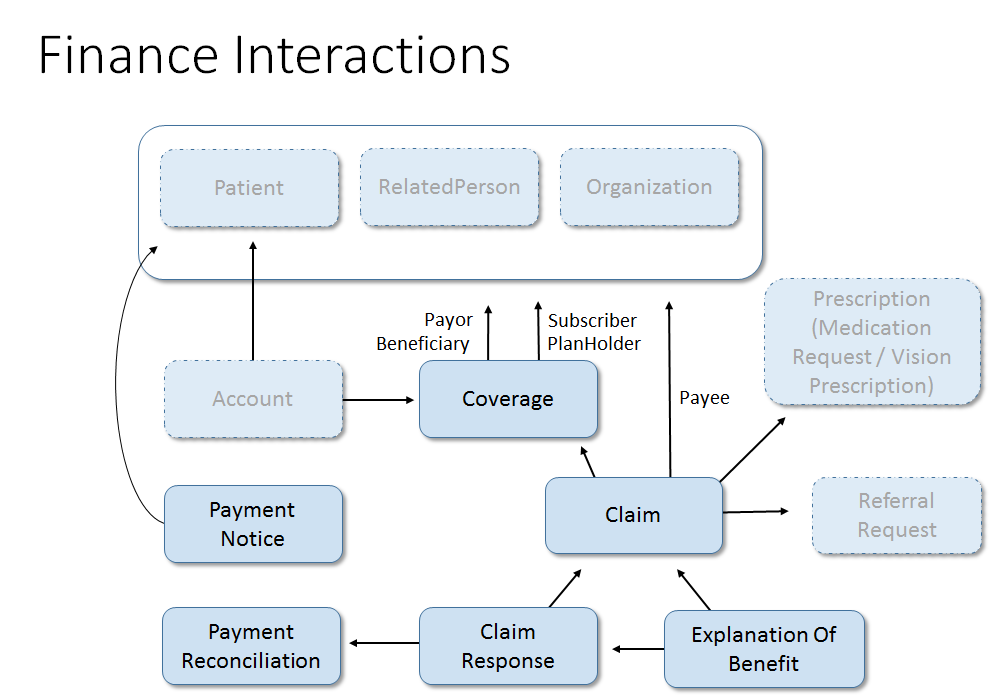
The Financial module covers the resources and services provided by FHIR to support the costing, financial transactions and billing which occur within a healthcare provider as well as the eligibility, enrollment, authorizations, claims and payments which occur between healthcare providers and insurers and the reporting and notification between insurers and subscribers and patients.
See also the Administration and WorkFlow modules.
Administrative
| Name | Aliases | Description |
| Account | Cost center | A financial tool for tracking value accrued for a particular purpose. In the healthcare field, used to track charges for a patient, cost centers, etc. |
| Coverage | Financial instrument which may be used to pay for or reimburse health care products and services. | |
| EligibilityRequest | This resource provides the details from the insurer to identify a specified coverage and optionally some class of service. | |
| EligibilityResponse | This resource provides eligibility and plan details from the processing of an Eligibility resource. | |
| EnrollmentRequest | This resource provides the insurance enrollment details to the insurer regarding a specified coverage. | |
| EnrollmentResponse | This resource provides enrollment and plan details from the processing of an Enrollment resource. |
Claims, processing and responses
| Name | Aliases | Description |
| Claim | A provider issued list of services and products provided, or to be provided, to a patient which is provided to an insurer for payment recovery. | |
| ClaimResponse | Remittance Advice | This resource provides the adjudication details from the processing of a Claim resource. |
Used to support service payment processing and reporting
| Name | Aliases | Description |
| PaymentNotice | This resource provides the status of the payment for goods and services rendered, and the request and response resource references. | |
| PaymentReconciliation | This resource provides payment details and claim references supporting a bulk payment. |
Patient reporting and other purposes
| Name | Aliases | Description |
| ExplanationOfBenefit | EOB | This resource provides: the claim details; adjudication details from the processing of a Claim; and optionally account balance information, for informing the subscriber of the benefits provided. |
Additional Resources will be added in the future. A list of hypothesized resources can be found on the
HL7 wiki  . Feel free to add any you think are missing or engage with one
of the HL7 Work Groups
. Feel free to add any you think are missing or engage with one
of the HL7 Work Groups  to submit a
proposal
to submit a
proposal  to define a resource of particular interest.
to define a resource of particular interest.
Financial information in general and in particular when related to or including health information, such as claims data, are typically considered Protected Health Information and as such must be afforded the same protection and safeguards as would be afforded to purely clinical identified health data.
The Security and Privacy measures associated with FHIR, such as the use of Security labels and tags in the resource.meta, is encouraged as are the use of whatever measures for authorization and encryption are supported by the chosen exchange model, eg. FHIR REST, Web Services, Direct, MLLP, SMTP and others.
For more general considerations, see the Security and Privacy module.
The table below details various common business activities which occur in the financial realm, and the focal resources which may be exchanged, along with supporting resources, to accomplish the business activities. Whether or not the resources specified are actually needed requires consideration of the business itself and the exchange methodology and transport being used.
For example, if a definitive 'Request' does not need to be documented and communicating parties are using FHIR REST then a Read or Search (GET) may be used in place of a Create (POST) of the request resource. Alternately, if FHIR Operations are being used then the specified focal resource may be employed as one of the Operation parameters or may not be required.
| Business Activity | Request Resource | Response Resource |
| Eligibility Check | EligibilityRequest | EligibilityResponse |
| Enrollment Update | EnrollmentRequest | EnrollmentResponse |
| Claim | Claim (type={discipline}, use=complete) | ClaimResponse |
| Pre-determination | Claim (type={discipline}, use=exploratory) | ClaimResponse |
| Pre-Authorization | Claim (type={discipline}, use=proposed) | ClaimResponse |
| Reversal | ProcessRequest (action=cancel, nullify=false) | ClaimResponse |
| Nullify | ProcessRequest (action=cancel, nullify=true) | ClaimResponse |
| Re-adjudication | ProcessRequest (action=reprocess) | ClaimResponse |
| Status Check | ProcessRequest (action=status) | ProcessResponse |
| Pended Check (Polling) | ProcessRequest (action=poll) | {Resource} or ProcessResponse |
| Payment Notice | PaymentNotice | ProcessResponse |
| Payment Reconciliation | ProcessRequest (action=poll, include=PaymentReconciliation) | PaymentReconciliation |
| Send Attachments | Communication | ProcessResponse |
| Request Attachments | ProcessRequest (action=poll, include=CommunicationRequest) | CommunicationRequest |
| Request an Explanation of Benefits | ProcessRequest (action=poll, include=ExplanationOfBenefit) | ExplanationOfBenefit |
{discipline} means the type of claim: OralHealth, Vision, Pharmacy, Professional or Institutional.
{Resource} means any pended or undelivered resource subject to the selection details specified in the request.
The table below details the relative order of events and use of financial resources for patient care during the care cycle. Not all steps or information exchanges may occur, and supporting information may be required more frequently than has been depicted below.
| Business Activity | Focal Resource |
| Patient visits Provider | |
| Provider checks for valid insurance coverage | EligibilityRequest |
| Insurer responds with coverage status and optional plan details | EligibilityResponse |
| Provider examines Patient and reviews treatment options | |
| Provider submits Pre-determination(s) for treatment options to determine potential reimbursement | Claim {use=exploratory} |
| Insurer responds with potential reimbursement | ClaimResponse |
| Provider and Patient determine treatment plan | |
| Treament plan submitted to Insurer to reserve funds | Claim {use=proposed} |
| Insurer acknowledges receipt of pre-authorization | ClaimResponse |
| Insurer requests additional information | CommunicationRequest |
| Provider submits supporting information | Communication |
| Insurer provides adjudicated response to pre-authorization | ClaimResponse |
| Provider checks on status of pre-authorization processing | ProcessRequest {action=status} |
| Insurer responds indicating adjudication is ready | ProcessResponse |
| Provider retrieves pre-authorization adjudication | READ or ProcessRequest {action=poll} |
| Provider provides treatment | |
| Provider submits patient's claim for reimbursement | Claim {use=complete} |
| Insurer responds with claim adjudication | ClaimResponse |
| Patient leaves treatment setting | |
| Patient requests an Explanation of Benefit for their Personal Health Record application | READ or ProcessRequest {action=poll} |
| Insurer responds with Explanation of Benefit | ExplanationOfBenefit |
| Provider requests the payment details associated with a bulk payment | SEARCH or ProcessRequest {action=poll} |
| Insurer responds with a Payment Reconciliation | PaymentReconciliation |
| Insurer notifies provider that payment has been issued | PaymentNotice |
| Insurer notifies parties that payment funds have been received | PaymentNotice |
In addition to their primary use of conveying patient billing information to insurers for reimbursement either to the subscriber or the provider (assignment of benefit), many of the financial resources, such as Claim and ExplanationOfBenefit, may be used to export data to other agencies to support reporting and analytics.
There is often a need to provide supporting information, commonly referred to as attachments, to document the need for a service and/or to confirm that the good or service was actually authorized or rendered. This information may be in many forms, including: scanned documents, PDFs, word processing files, XRays, images, CDAs and FHIR Resources.
Supporting information may be provided, as a reference or the actual material, to support the Claim (complete claim or Pre-Authorization) or ExplanationOfBenefit in a variety of manners:
The Financial Management Work Group (FM) is responsible for two subdomains:
Financial Accounts and Billing (FIAB) - resources for accounts, charges (internal costing transactions) and patient billing, and
Financial Claims and Reimbursement (FICR) - insurance information, enrollement, eligibility, pre-authorization, claims, patient reporting and payments.
To date FM has been focusing on the resources required to support the exchange of claims and related information between healthcare providers and insurers. The first draft of this work is nearing completion with the release of the first Financial Standard for Trial Use in STU3 of FHIR. Over the next year further refinements will be expected as we begin developing regional profiles and begin live pilots with resources.
Once the above is well underway FM can then look to developing the Enrollment-related resources and the resources to support the FIAB functions.