This page is part of the Consumer Real-time Pharmacy Benefit Check (v0.1.0: STU 1 Ballot 1) based on FHIR R4. The current version which supercedes this version is 1.0.0. For a full list of available versions, see the Directory of published versions 
Information content and FHIR resources
The real-time pharmacy benefit check (RTPBC) process involves a request from a consumer application used by a patient to either (a) the party that manages the pharmacy benefit portion of the patient’s health insurance or (b) a party that serves as a source for typical and discount medication pricing information.
Content when submitting to the patient’s insurer
Request content
The patient application submits a request containing…
- basic patient identifying information
- payer and coverage identifiers
- information from the prescription for which coverage and cost is desired
- the patient’s preferred pharmacy
Example: Bundled RTPBC request
Response content
The responder…
- locates the patient’s record and coverage details
- determines the patient’s out of pocket cost for the requested pharmacy and potentially other pharmacy options
- determines if alternative medications are available and identifies coverage and cost for those
- returns the gathered information to requester
Example: Bundled RTPBC response from payer/PBM
Content when submitting to a medication pricing source
Request content
The patient application submits a request containing…
- information from the prescription for which pricing is desired
- the patient’s location and preferred pharmacy
Response content
The responder…
- determines pricing for the requested pharmacy and potentially other nearby pharmacies, including discounts associated with coupons or memberships
- returns the gathered information to requester
Resources used in the exchange
The consumer RTPBC request and response are accomplished using FHIR® Claim and ClaimResponse resources in a “predetermination” (what-if) mode. Other FHIR® resources support the exchange by fleshing out patient, prescription, pharmacy and coverage information needed to determine accurate cost and coverage. An OperationOutcome communicates exception situations where a ClaimResponse cannot be returned
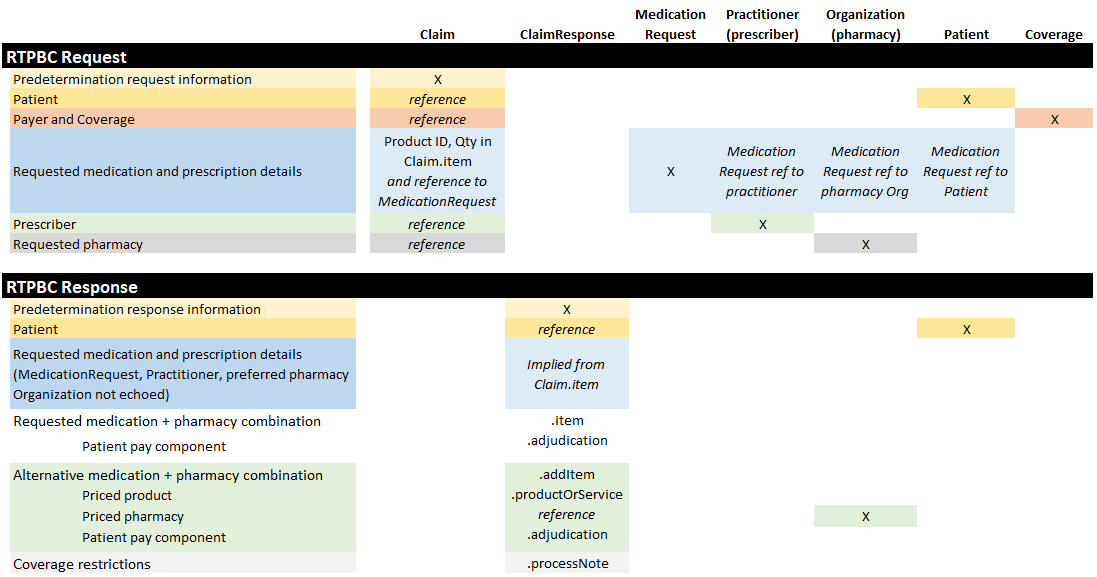
Below are profiles constraining those resources for this purpose:
- Claim - Represents the RTPBC request. Uses the predetermination Claim.use mode
- ClaimResponse - Represents the RTPBC response
- Patient - Conveys the patient information needed for the exchange
- MedicationRequest - Conveys the needed prescription information (a subset of what is present in a full prescription)
- Practitioner - Conveys the prescriber information needed for the exchange
- Organization (Pharmacy) - Conveys pharmacy information needed for the exchange
- Coverage - Conveys the patient’s pharmacy benefit coverage IDs



