This page is part of the Validated Healthcare Directory FHIR IG (v0.1.0: STU 1 Draft) based on FHIR (HL7® FHIR® Standard) v3.2.0. The current version which supersedes this version is 1.0.0. For a full list of available versions, see the Directory of published versions
This section outlines important definitions and interpretations used in the Validated Healthcare Directory IG. The conformance verbs used are defined in [FHIR Conformance Rules].
Contents
The VHDir IG provides a specification for the exchange of data from a national source of validated provider information to organizations implementing healthcare directories to satisfy their own, local use cases.
Must Support on any data element SHALL be interpreted as follows:
Validated Healthcare Directory Requestors SHALL be able to process resource instances containing data elements asserting missing information.
A practitioner is a person who is directly or indirectly involved in the provisioning of healthcare.
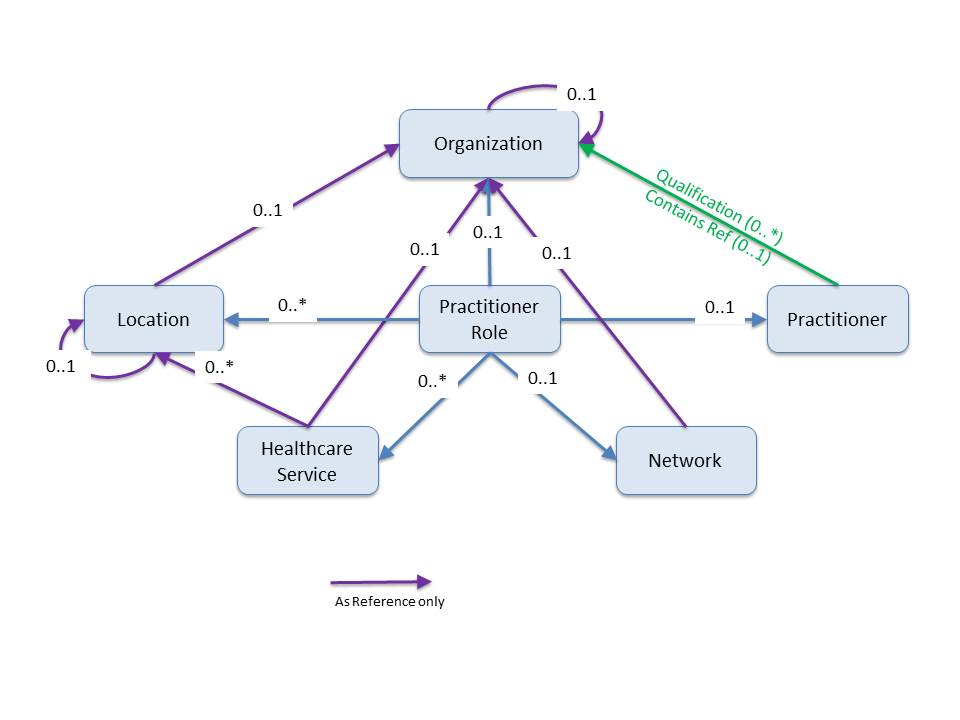
PractionerRole describes the relationship between a practitioner and an organization. A practitioner provides services to the organization at a location. Practitioners also participate in healthcare provider insurance networks through their role at an organization.
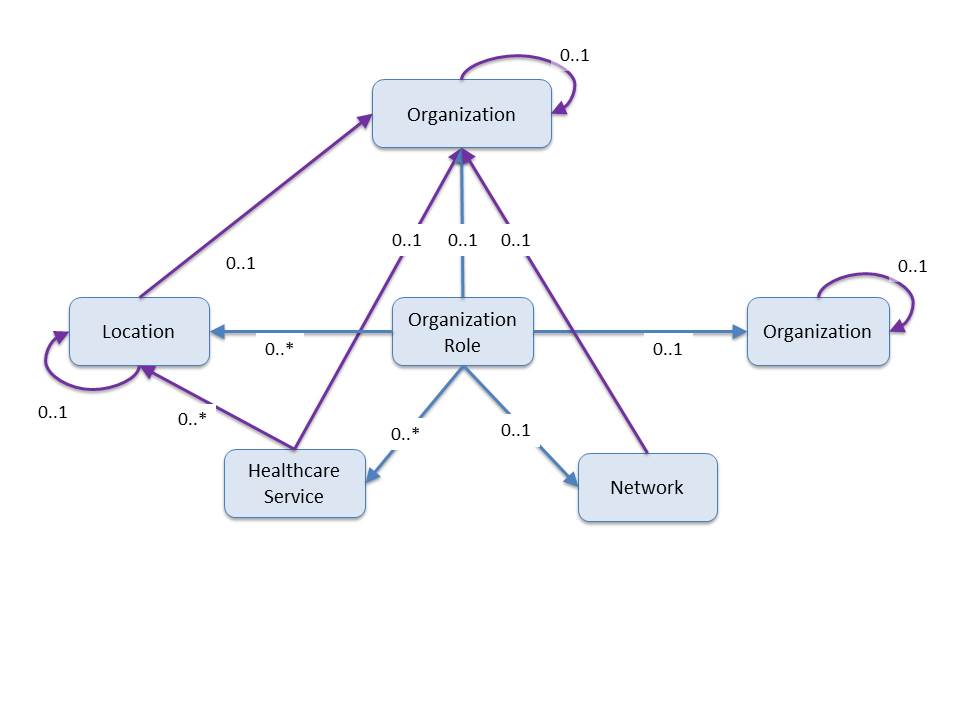
Similar to practitionerRole, OrganizationRole describes relationships between organizations. For example: 1) the relationship between an organization and an association it is a member of (e.g. hospitals in a hospital association), 2) an organization that provides services to another organization, such as an organization contracted to provide mental health care for another organization as part of a healthcare provider insurance network, and 3) distinct organizations forming a partnership to provide services (e.g. a cancer center).
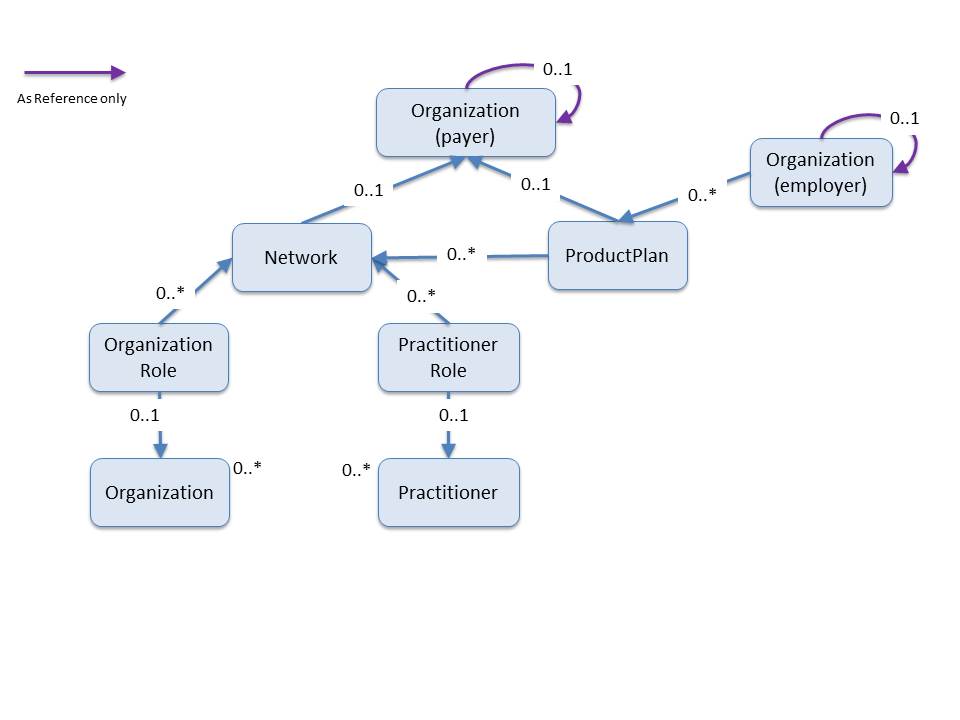
A network is a group of practitioners and organizations that provide healthcare services for individuals enrolled in a health insurance product/plan (typically on behalf of a payer).
Extensible binding to a value set definition for this IG means that if the data type is CodeableConcept, then one of the coding values SHALL be from the specified value set if a code applies, but if no suitable code exists in the value set and no further restrictions have been applied (such as the max valueset binding described in the next section), alternate code(s) may be provided in its place. If only text available, then just text may be used.
Example: Product/Plan’s coverage type coding - the source only has the text “4-way Influenza” and no coverage type code.
{ “resourceType”: “productPlan”, … “coverage.Type”: { “text”:”orthodontics - extended” }, … }
For this IG, we have defined the Extensible + Max-ValueSet binding to allow for either a code from the defined value set or text if the code is not available. (for example, legacy data). This means, unlike a FHIR extensible binding, alternate code(s) are not permitted and a text value SHALL be supplied if the code is not available. However, multiple codings (translations) are allowed.
Required binding to a value set definition for this IG means that one of the codes from the specified value set SHALL be used. If only text is available or the local (proprietary, system) code cannot be mapped to one of the required codes the [core specification] provides guidance which we have summarized:
Note that when a query uses a status parameter, a status will be ambiguous.
Example: Endpoint resource with a status that is text only or cannot be mapped to the status value set.
\{
"resourceType”:“Endpoint”,
...
“\_status”:{
“url” : “http://hl7.org/fhir/STU3/StructureDefinition/data-absent-reason”,
“valueCode” : “unsupported”
...
},
}
Required binding to a value set definition means that one of the codes from the specified value set SHALL be used and using only text is not valid. In this IG, we have defined the Extensible + Max-ValueSet binding to allow for either a code from the specified value set or text. Multiple codings (translations) are permitted as is discussed below.
Alternate codes may be provided in addition to the standard codes defined in required or extensible value sets. The alternate codes are called “translations”. These translations may be equivalent to or narrower in meaning to the standard concept code. <!– Example of multiple translation for Body Weight concept code.
"code": {
"coding": [
{
"system": "http://loinc.org", //NOTE:this is the standard concept defined in the value set//
"code": "29463-7",
"display": "Body Weight"
},
//NOTE:this is a translation to a more specific concept
{
"system": "http://loinc.org",
"code": "3141-9",
"display": "Body Weight Measured"
},
//NOTE:this is a translation to a different code system (Snomed CT)
{
"system": "http://snomed.info/sct",
"code": “364589006”,
"display": "Body Weight"
}
//NOTE:this is a translation to a locally defined code
{
"system": "http://AcmeHealthCare.org",
"code": “BWT”,
"display": "Body Weight"
}
],
"text": "weight"
},
Example of translation of CVX vaccine code to NDC code.
"vaccineCode" : {
"coding" : [
{
"system" : "http://hl7.org/fhir/STU3/sid/cvx",
"code" : "158",
"display" : "influenza, injectable, quadrivalent"
},
{
"system" : "http://hl7.org/fhir/STU3/sid/ndc",
"code" : "49281-0623-78",
"display" : "FLUZONE QUADRIVALENT"
}
]
},
!–>
Interactions on profile pages are defined with the syntax:
GET [base]/[Resource-type]/[id] {parameters}
For more information see the [FHIR RESTful API]
In the simplest case, a search is executed by performing a GET operation in the RESTful framework:
GET [base]/[Resource-type]?name=value&…
For this RESTful search ([FHIR Search]), the parameters are a series of name=[value] pairs encoded in the URL. The search parameter names are defined for each resource. See [FHIR Search] for more information about searching in REST, messaging, and services.
There are several potential ways to search for resources associated with a specific practitioner depending on the context and implementation. These searches result in the same outcome.:
There are several variations to this syntax which are listed below:
Validated Healthcare Directory servers are not required to resolve full URLs that are external to their environment.
In order to manage the number of search results returned, the server may choose to return the results in a manner consistent with FHIR Bulk Data Access Standards. For a simple RESTful search, the page links are contained in the returned bundle as links. See the [FHIR Paging] (https://www.hl7.org/fhir/http.html#paging) and [Bulk Data Aceess] (http://www.healthintersections.com.au/?p=2689) for more information.