This page is part of the National Healthcare Directory Exchange (v1.0.0-ballot: STU 1 Ballot 1) based on FHIR (HL7® FHIR® Standard) R4. No current official version has been published yet. For a full list of available versions, see the Directory of published versions
Contents
Healthcare directories play a critical role in enabling identification of individual providers and provider organizations, as well as characteristics about them, their relationships, and the means by which to access and exchange health information among them electronically. Healthcare directories support a variety of use cases, including:
Today, many healthcare organizations maintain directories, including providers, payers, health information exchange organizations (HIEs/HIOs), health information service providers (HISPs), government agencies, and credentialing organizations. However, despite their importance, healthcare directory activities remain scattered, uncoordinated, and are often not interoperable. As a result, the healthcare industry collectively spends significant time and resources registering and validating demographic information for individual and organizational providers for purposes such as licensure, credentialing, certification, and payment.
Providers often have to submit and manage information about themselves and their places of employment to a variety of stakeholders. In the US, providers often contract with ten or more health plans, and are required to regularly submit similar information to each plan for inclusion in a provider directory. Likewise, provider credentialing and hospital privileging processes require similar documentation. The Council for Affordable Quality Healthcare has estimated that maintaining provider databases costs the US healthcare industry at least $2 billion annually.
Due to the high cost of acquiring and maintaining provider information and keeping it current, existing healthcare directories often contain information that is inaccurate, out of date, or not validated.
This implementation guide uses the term ‘healthcare directory’ instead of ‘provider directory’ because it encompasses all individuals and entities that provide services which may impact an individual’s health and well-being. We did not limit the definition of a directory to include only those individuals/entities that are licensed to practice medicine and/or bill for healthcare services. Rather, a validated healthcare directory may include data about community/social service entities and non-licensed administrative/support staff, among others.
Patient/caregiver information, however, is considered out of scope for a VHDir.
On April 5th and 6th, 2016, the Office of the National Coordinator for Health Information Technology (ONC) and the Federal Health Architecture (FHA) jointly hosted a Provider Directory Workshop to convene public and private stakeholders to review challenges, share successes, and generate new ideas around provider directory standards and solutions. Although participants described different use cases for healthcare directories, they agreed that provider data quality is a persistent challenge across the industry.
To address concerns about data quality, reduce administrative burden, and improve consumer satisfaction, ONC and FHA launched a new healthcare directory effort in July 2016. The project sought to: (1) define the architecture of a central source of validated healthcare directory data, and (2) develop a Fast Healthcare Interoperability Resources (FHIR) Implementation Guide describing the exchange of information between a central source of validated healthcare directory data and local environments (e.g. provider organizations, payers, HIEs).
Such a central source would include a broad set of provider data to support a variety of healthcare directory use cases. Data would be validated against primary sources (e.g. state licensing boards for licensure information) and available to local environments through a national FHIR-based exchange standard. Instead of submitting the same information to each payer and provider organization they worked with, providers would only have to attest to the majority of their information to the central source.
For more information on the ONC and FHA effort see the ONC Techlab Healthcare Directory Project
This implementation guide was written for an international audience. We expect different jurisdictions considering implementing a VHDir will design their implementations in accordance with jurisdictional requirements, such as national profiles/IGs. In the United States, for example, we expect a VHDir would align with an R4 version of the US Core IG once it becomes available.
To determine which resources to profile, extensions to create, etc. we reviewed a number of use cases supported by healthcare directories today:
For each use case, we described the general information requirements necessary to support the use case. We then specified the general information requirements as discrete data elements using FHIR resources. Therefore, this implementation guide covers a broad set of data elements supporting a range of use cases that may reasonably be collected, validated, and exchanged from a central source of validated provider data.
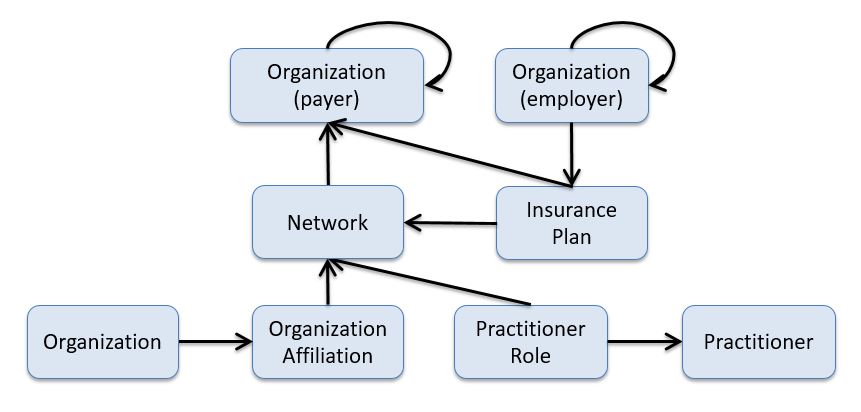
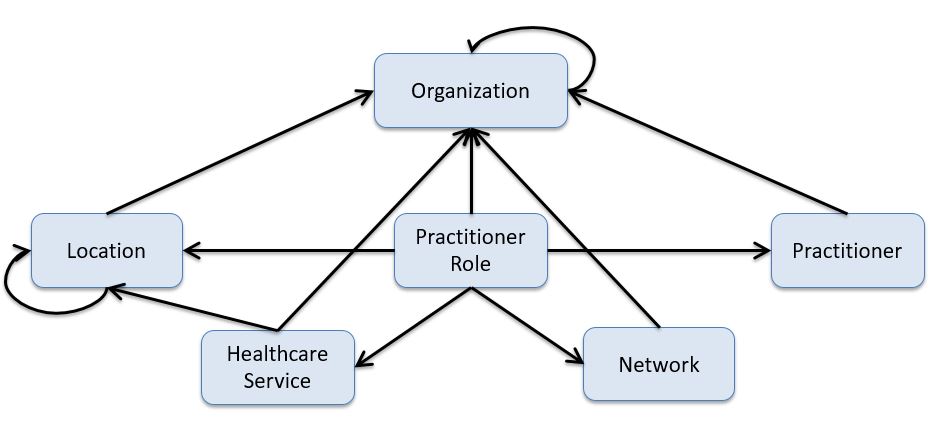
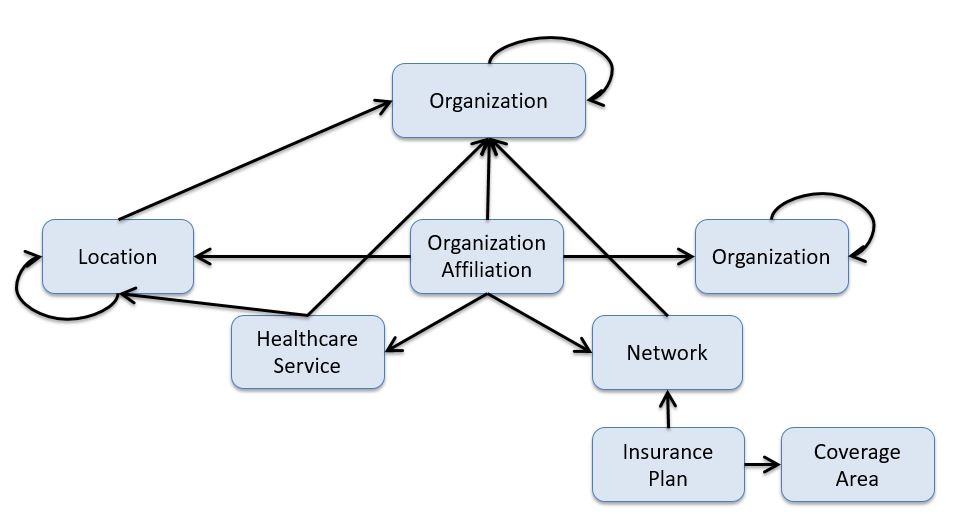
Note: the following diagrams provide a high-level view of the relationships between resources used in this IG. They do not necessarily reflect all of the relationships/references between resources.
A practitioner is a person who is directly or indirectly involved in the provisioning of healthcare.
PractionerRole describes the relationship between a practitioner and an organization. A practitioner provides services to the organization at a location. Practitioners also participate in healthcare provider insurance networks through their role at an organization.
Similar to PractitionerRole, OrganizationAffiliation describes relationships between organizations. For example: 1) the relationship between an organization and an association it is a member of (e.g. hospitals in a hospital association), 2) an organization that provides services to another organization, such as an organization contracted to provide mental health care for another organization as part of a healthcare provider insurance network, and 3) distinct organizations forming a partnership to provide services (e.g. a cancer center).
A network is a group of practitioners and organizations that provide healthcare services for individuals enrolled in a health insurance product/plan (typically on behalf of a payer).