This page is part of the Da Vinci Coverage Requirements Discovery (CRD) FHIR IG (v2.0.1: STU 2.0) based on FHIR (HL7® FHIR® Standard) R4. The current version which supersedes this version is 2.1.0. For a full list of available versions, see the Directory of published versions
| Page standards status: Informative |
Providers need to easily discover which payer covered services, medications (not covered by NCPDP) or devices have:
This implementation guide defines a FHIR based API that providers can use to discover, in real time, specific payer requirements that may affect whether services or devices provided to a patient are covered by their responsible payer. The Coverage Requirement Discovery may be based on:
When needed, the API will allow payers with authorization to query provider systems for additional patient information needed to inform the guidance provided - for example by determining what information already exists or what steps have already occurred.
The payer response to a CRD request might include:
Mrs. Jones is a 35-year-old, previously healthy female who is seen by Dr. Good for a new onset headache that began abruptly 2 weeks prior to her visit. Her headaches are severe at times, last several hours, have been occurring with increasing frequency, and are now occurring daily. Her physical including neurologic exam is normal. Dr. Good is concerned about an intracranial process.
Dr. Good wants to order a head CT to check for any masses. Dr. Good begins filling out the order for the CT in their EHR. In the background, the EHR initiates a call to the CRD Server used by Mrs. Jones’ payer providing information about the patient, her coverage and the CT order. The CRD service returns information within a few seconds identifying that a prior authorization request must be completed and submitted, as well as the additional clinical documentation required (Progress Note, prior studies, etc.). It also provides a link to the required form. Dr. Good launches an app to complete the necessary paperwork to initiate a prior authorization and sends the relevant supporting information to the imaging center as part of the referral.
Note: An app may also provide Dr. Good with additional useful information, such as a list of nearby imaging centers that are on Mrs. Jones’ plan.
Mrs. Smith is a 75-year-old female on a Medicare Fee-For-Service plan with long standing chronic obstructive pulmonary disease (COPD) who has had slowly and progressively worsening shortness of breath with activity. In the office, her room air saturation after a 5-minute walk is found to be 84%. She has additional evaluation that reveals no new findings. Dr. Good wants to initiate home oxygen therapy for Mrs. Smith.
Dr. Good is completing* an order for home oxygen therapy. The EMR initiates a query to the CRD Server used by her payer that includes the code for a portable oxygen generator. An alert appears on the EMR order entry screen notifying Dr. Good that specific testing and documentation is required to substantiate the need for a home oxygen therapy and specifically for a portable oxygen generator. The EMR allows Dr. Good to immediately document the required information by starting DTR.
DTR retrieves specific documentation templates which have already been populated with information from the EMR. Dr. Good completes the remaining documentation requirements that require clinical input, signs the documentation, and includes it in Mrs. Smith’s medical record. They leave the remaining portion of the documentation to be completed by their administrative staff who will find an appropriate supplier and forward the order and documentation.
* Note: This flow envisions the use of the Order Sign hook, which allows guidance to be returned while the user is in the process of signing the order.
Mr. Light is a 45-year-old generally healthy male who presents for an annual exam. His physical exam is normal. Dr. Good checks a basic metabolic panel and determines that Mr. Light’s kidney function is diminished (Creatinine of 2.5) which is new compared to his function one year prior (Creatinine of 1). Dr. Good wants to refer Mr. Light to a nephrologist for further evaluation.
As Dr. Good is completing the referral, their EMR contacts a CRD Server used by Mr. Light’s health plan. The service notifies him that, for the referral to be covered under Mr. Light’s coverage, the physician must request prior authorization and provide specific medication documentation as part of the request. The EMR provides a link to an insurer-provided app that displays the form, partly populated with information from their EMR and guides him through the process of completing the information needed for the prior authorization.
Mrs. Abdallah is a 30-year-old female who is struggling with weight issues. Dr. Good feels that she’d be a good candidate for a dietary consult, however Mrs. Abdallah isn’t sure whether her plan will cover the service and doesn’t think she can afford it on her current salary. Before going through the work of writing up a formal referral, Dr. Good opts to check whether a referral would be covered. They launch an app within their EHR which auto-populates with information from the current patient. They choose “MNT/nutrition counseling” from the list of possible referral services and the app contacts Mrs. Abdallah’s payer’s server. The server indicates that, while Mrs. Abdallah does have coverage, MNT/nutrition counseling is not a benefit of her plan. Dr. Good informs Mrs. Abdallah of this and they come up with an alternate plan. Dr. Good recommends a useful series of online videos and a couple of books Mrs. Abdallah can get from the library. He also suggests Mrs. Abdallah shop around a bit when it comes time to renew her coverage for the following year.
The high-level workflow for CRD is envisioned to work as follows:
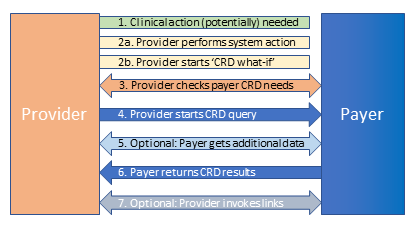
1. Clinical action (potentially) needed
A healthcare provider decides that a clinical action is needed or wants to explore the coverage ramifications of taking a clinical action. Possible clinical actions include:
Based on whether the provider has decided to perform the action or just wishes to explore, they will proceed to 2a or 2b.
2a. Provider performs EMR action
The provider uses an EMR to initiate the clinical action from step #1, entering required information (e.g. a drug, a type of referral or appointment, etc.) into forms provided by the EMR.
2b. Provider starts ‘CRD what-if’
The provider uses an EMR to launch a ‘What if?’ CRD SMART app to explore payer coverage requirements. The provider indicates the type of action they’re considering into the CRD SMART app which prompts for additional information relevant to coverage determination, such as the proposed drug, type of referral or appointment, etc.
3. Provider checks Payer CRD needs
The EMR or CRD SMART app contacts a CRD Server used by their patient’s payer to find out what information is required to perform Coverage Requirements Discovery (CRD) - particularly whether the CRD Server requires protected health information (PHI) to evaluate the patient’s coverage requirements, or whether the patient’s coverage type and the proposed clinical action is enough. Optionally, the CRD service might provide the EMR with information about configuration options, such as the option to control the types of coverage requirements returned to the user or the number of requirements returned.
Note:
It is up to payers to determine whether and how long to cache information such as “is member covered” and “what are coverage rules for service x”, as well as if and how to check whether cached information is ‘dirty’ (i.e. the underlying record has changed). From a performance perspective, if follow-on hooks (i.e. Order Dispatch or a subsequent Order Sign for revisions) are invoked, there is no expectation information will be cached if no hook for that patient have fired in the last 24 hours, which is why the response time target is longer in that situation.
In the event decisions are made based on ‘dirty’ cached data, the unique identifier provided with the Coverage Information extension will allow the payer to trace what information the decision was based on. In general, if a decision is based on information outside the payer’s control (e.g. a policy being cancelled), they will not be held to the decision conveyed to the CRD client. If a decision is based on changes within the payer’s control (e.g. rules for when prior authorization is needed have changed), payers are expected to respect the decision that was conveyed to the CRD client.
4. System starts CRD query
The EMR (in the background as the provider is typing) or the CRD SMART app (once enough information has been provided) initiates a query to the CRD Server providing the patient’s coverage type and/or identity along with information about the proposed clinical action. The EMR might also provide the CRD Server with one or more of the following:
Note:
5. (Optional) Payer service gets additional data
If additional information is needed to process the query, the CRD Server may use the EMR’s secure API, with the temporary access token provided in step #4, to request additional information from the patient’s record. (In some cases, the EHR may provide information up-front based on pre-fetch requests from the payer’s configuration information.) Examples include requests for information needed to assess whether the action is needed (e.g. an allergy to a first line medication, lab result), whether recommended next steps are in place (e.g. follow-up visits scheduled, lab tests ordered to monitor effectiveness/safety), etc. The CRD Server might submit multiple queries for different types of data to determine coverage requirements.
Note:
6. Payer service returns CRD results
Based on the information provided/retrieved, the payer system returns guidance to the provider. The guidance can be in several forms:
Payer requirements might include the need for prior authorization, forms that must be completed, medical documentation that must exist or be provided, recommendations on alternative therapies, etc.
7. Provider invokes links
If the response includes links to additional information or apps, the provider can direct the EMR to interact further with the payer system by retrieving the linked-to information or launching the provided application.
While the primary purpose of this implementation guide is to ensure that healthcare providers using EMRs are aware of insurance plan requirements that might impact payment for services rendered, the CRD architecture and infrastructure can potentially be used for other purposes that enhance the provider-payer-patient relationship: